Definitive diagnosis and control of axillary hyperhidrosis (excessive sweating of the armpit area)
Certain diagnosis and control of excessive underarm sweating
with curettage and suction method
Abstract
Background: Excessive axillary sweating is a benign yet significant disability that affects not only social interactions but also occupational activities.
Objectives: The researcher and author of the following article provides a detailed description of the surgical method of shaving the sweat glands in the armpit area, a method with proven results. He also describes the use of an evapometer (VapoMeter manufactured by Delfin Technologies, Stamford, Connecticut), which easily and accurately measures the amount of perspiration in g/m2/h (gram/square meter/hour).Methods used: Although a total of 45 patients have undergone this surgery since 2005, this report only includes the last eight patients (16 cases of axillary surgery) whose pre- and post-operative evaporimeter interpretations are available.
Findings: The average interpretation of evapotranspiration before the operation was 473 g/m2/h (range 998-98), which improved to an average of 58 g/m2/h (range 227-21) after the operation. As a comparison, the control rate for the entire axillary area measured an average of 23.7 g/m2/h (range 18-31).
Conclusion: By combining the effective surgical technique of underarm shaving, the vaporizer provides objective and real measurements for accurate diagnosis and confirmed results of shaving. With the help of this protocol, hyperhidrosis patients who need surgical intervention can ensure that this process is actually effective in improving their conditions.
Keywords:
Hyperhidrosis, armpit shaving surgery, eccrine glands, sweat, perspiration, evapotranspiration
Hyperhidrosis is defined as excessive sweating beyond the normal physiological response to heat or emotional stimuli. Usually, when the body is overheated, the sweat glands are stimulated and produce moisture with a cooling effect due to evaporation. When the amount of sweat is produced more than a person's physiological needs, severe social, psychological or occupational disorders may occur. Normal values are defined as less than 1 mL/m2/min. In patients with acute profuse sweating, sweat production can even exceed 40 mL/m2/min. Qualitatively, it can be said that any type of sweating that negatively affects people's daily lives and compromises their natural interactions with the world around them is considered excessive.
The highest density of eccrine glands (sweat production) is in the palms, armpits and soles of the feet. Only about 5% of these glands are normally active at the same time, but there is a high potential for excessive sweat production in any of these areas. The number of apocrine glands in the axillary and urogenital areas is less; They are activated during puberty; These glands are hidden and secreted in the hair follicles and produce a sticky and fragrant liquid. In case of excessive secretion, it causes a strong and unpleasant smell (asmidrosis or severe armpit odor disease/bromidrosis). The condition is most commonly reported in the Far East, where it causes as much social disability as hyperhidrosis. A third of recent reports are related to apo-eccrine glands, which are only seen in adults and share morphological (structural) and functional features with both apocrine and eccrine glands. These glands are similar in texture to apocrine glands, except that they are secreted and discharged to the axillary surface.
To see the video clip of the surgery, scan this code with your smartphone with the barcode scanner app.

Table 1
Common diseases and conditions associated with excessive sweating
| Acute febrile illness |
| Alcohol addiction |
| Diabetes |
| Gout |
| heart failure |
| Hyperthyroidism |
| Lymph node cancer |
| menopause |
| Additional weight |
| Parkinson's disease |
| Pregnancy |
| Rheumatoid arthritis (rheumatism of the joints) |
| drug abuse |
Table 2. Classification of commonly known drugs that can cause excessive sweating
| Painkillers and sedatives, medtomidine |
| Anti-infective drugs |
| cardiovascular drugs |
| Chemotherapy drugs |
| skin medicines |
| Drugs related to endocrine diseases |
| digestive drugs |
| medicines related to head and neck diseases |
| Medications related to blood disorders |
| nerve and psychoactive drugs |
| Medicines for eye diseases |
| Drugs for lung diseases |
| Drugs for urological diseases and urinary system |
These unique glands are not located in the interdermal layer, but in the subcutaneous tissue of the axillary region, and this fact is of particular importance when considering the explanation and cause of the effectiveness of axillary shaving in the treatment of axillary hyperhidrosis.
The causes of excessive sweating can generally be divided into two broad categories: primary (for which there is no identifiable cause) and secondary (which can result from a host of causes listed in Tables 1 and 2). This report focuses on primary hyperhidrosis, a disease with no known cause. This type of hyperhidrosis is considered as an idiopathic or unknown disease and is related to the excessive production of sweat by eccrine glands (sweating) or the production of abnormal body odor by apocrine glands (bromidrosis or strong body odor).
Although hyperhidrosis was considered a benign and unimportant condition for many years, it is now recognized as a very debilitating factor because it can harm the interactions and social and occupational activities of the affected person. In addition to its unnatural function, it is much more common than before. According to a recent American survey, 2.8% of the population (8 million people) suffer from systemic hyperhidrosis (excessive sweating of the face, armpits, palms, or feet); This case includes 1.4% of the population with severe symptomatic armpit sweating. A study on a third of people with axillary hyperhidrosis showed that sweating is intolerable or barely tolerable to the extent that their daily activities are often or always disrupted by reducing the time they spend for leisure or work. Patients go through a significant long-term process of adjusting their lives to overcome the appearance or smell of armpit sweat in order to hide their condition.Hyperhidrosis or excessive sweating in work conditions creates disorders and potential problems in grasping, holding and holding tools or paper; Also, the person has to change his clothes many times.
These things, in turn, strongly affect career choices; In jobs related to education, sales and marketing, it creates restrictions or removes them altogether.
Jobs that include paper, metal, and electrical or electronic equipment are just as unattainable as the jobs mentioned. This condition in itself is not a limitation, the patients are mostly dealing with emotional distress and despair of dealing with the inability to control normal life.In short, quality of life (QOL) in all areas can be significantly affected by these conditions.
The importance of this problem is confirmed by QOL scales showing that hyperhidrosis is comparable to advanced kidney disease, rheumatoid arthritis (rheumatism of the joints), multiple sclerosis, and severe psoriasis. Recent data show that family history can have an effect on this problem and almost half of patients with it have reported a positive family history. This disease is related to chromosomes. It is slightly more common in women than men and often occurs before the age of 25, although the condition is said to develop at birth. There is no ethnic or sociological affiliation and relevance in creating these conditions.
Patient examination and diagnosis
The patient and the doctor may not succeed in diagnosing primary hyperhidrosis as a common and treatable disease. As part of charting the patient's history, the anatomic site(s), frequency, duration, previous lifestyle changes, family history, comorbidities, and use of drugs known to induce sweating should all be identified.
However, note that there is usually less moisture on physical examination than the affected area. Primary hyperhidrosis is defined as focal or localized, visible and excessive sweating for a period of at least six months without apparent cause and having at least two of the following features:
- Two-sided and relatively symmetrical areas
- Disturbance in daily activities

Figure 1. Hand-held evaporimeter (Delfin Technologies Stamford, Connecticut).
Recurrence of excessive sweating at least once a week
- Age of onset less than 25 years (often in the teenage years)
- Positive family history
- Stop focal sweating during sleep
Until recently, there were only three ways to diagnose primary focal hyperhidrosis:
(1) gravimetric test (literally means measuring moisture on a filter paper, which is tedious and impractical in clinical cases); (2) starch and iodine test, which involves placing starch and iodine in the target area (if a black-purple color appears within 5 minutes, the test is considered positive, but the results are not necessarily reproducible and the test lacks objectivity); or (3) the ninhydrin test, based on the principle that ninhydrin reacts with the amino acids in sweat, and by creating this effect, enables measurement through digital analysis of the image or effect created on the paper.
Another way to evaluate the importance of hyperhidrosis in a patient is the severity index of hyperhidrosis disease.
This hyperhidrosis questionnaire is designed to evaluate how patients determine the effect of sweat on their daily activities. Responses are presented on a four-dimensional scale: (1) = not significant at all, does not interfere at all; (2) = tolerable, sometimes interferes (3) = barely tolerable, often interferes and (4) = intolerable, always interferes.
A high score indicates a severe impact on QOL. This scale should be administered before starting any treatment and is used as a means of determining the potential effect of treatment. If the patient feels that the treatment has improved by one level (i.e., from "4" to "3"), we will see a 50% reduction in sweating, while an improvement of two levels correlates with an 80% reduction in sweating.
During the last few years, another method has been reported to measure TEWL or the amount of water that evaporates from the surface of the skin over a period of time (g/m2/h).
VapoMeter (Stamford, Connecticut VapoMeter, Delfin Technologies,) provides a practical and verifiable method for rapid evaluation of TEWL, in fact within 10 seconds (Figure 1).
Although this tool has been used in the cosmetic and antiperspirant industry for many years, it has only recently been used to assess excessive sweating in the palm area.
There have been no previous reports of its use for axillary hyperhidrosis, but it has objectively demonstrated TEWL before and after bilateral thoracoscopic sympathectomy.
Non-surgical control of severe underarm sweating
Many treatments have been proposed to control excessive sweating, suggesting that there is no specific method that works for all patients. Because of their availability, safety, affordability, and effectiveness, first-line nonsurgical treatments include over-the-counter ointments or antiperspirants, followed by topical antiperspirants and clinical-grade, prescription oral medications.
All these precautions should be taken before exposure to more invasive treatments.
The most common prescribed topical antiperspirant is Drysol (Person & Covey, Glendale, California), a proprietary formula of aluminum chloride hexahydrate, but this treatment has disadvantages such as its relatively short-term effect (3 to 5 days), as well as local skin irritation.
Another topical antiperspirant with a lower concentration of aluminum chloride with 2% salicylic acid called Hydrosal (Valeo Pharma, Corp, Kirkland, Quebec) has recently been introduced to the market and appears to be as effective as Drysol, but with less burning and sensitivity of the axillary skin. This product is only available on the Internet, and does not require a prescription.
Oral anticholinergic agents (i.e. glycopyrrolate) can be effective, but have potentially troublesome and dangerous side effects, including dry mouth, blurred vision, hypotension, and tachycardia (heart palpitations). Also, their use has side effects such as angle closure glaucoma, gastric reflux and heart failure.
Another non-surgical treatment is iontophoresis, in which the direct passage of galvanic current is done through the skin immersed in water. Although in focal areas, such as hands or feet, it is not logically satisfactory in the case of heavy sweating in the armpit area.
Finally, the injection of botulinum toxin type A inhibits the release of acetylcholine at the junction of sympathetic neuromuscular and cholinergic nerve endings that stimulate the eccrine sweat glands, thereby reducing sweat production. Although botulinum type A is predictably effective, it only lasts four to six months. However, this treatment will be elective for areas or conditions that cannot be treated with surgery (eg head and face, Frey's syndrome or postprandial sweating, etc., plantar fascia) or for those who are unable or unwilling to undergo invasive surgery.
Surgical management of severe axillary sweating
When non-surgical methods are not effective in the armpit area, surgical intervention should be considered.

Figure 2. The axillary hair is shaved and defined. A 1 cm access incision is marked in the anterior part of the midline of the axillary region.
Local methods include different types of axillary excision, which include cutting and removing all skin and subcutaneous tissue, original subcutaneous tissue through incision without any actual skin cutting and removal, total or partial skin excision with open subcutaneous tissue removal, laser gland destruction and curettage, and liposuction.
The degree of success of these techniques varies, but there are still irritations such as unacceptable morbidity associated with axillary ulcers, hematoma formation, skin necrosis, and limitation of hand and arm movements. Endoscopic thoracic sympathectomy has also been suggested as a very effective surgery for palmar hyperhidrosis.
Previously, the results of all these techniques have been assessed through direct patient responses or postal questionnaires, both of which are subjective and lack objective reproducibility. An article by Tang showed good results in the treatment of axillary hyperhidrosis using the arthroscopic shaver technique. Independently, Arenja et al have reported a similar technique for axillary hyperhidrosis with excellent results. This method (also described here), when combined with the objective measurement provided by the evaporimeter, will provide permanent relief and relief from the disability of a patient with axillary hyperhidrosis. Since 2005, this researcher has used the arthroscopic shaver technique to treat axillary hyperhidrosis, like previous researchers, and has found it very effective. Recently, however, the success of this method is based only on subjective and personal information of patients. In April 2009, an evaporimeter was made available in the researcher's clinic, which enabled him to objectively measure water evaporation in g/m2/h. Here, the results of a series of patients treated with both methods of using a vaporizer and shaving the armpit area are reported.
Methods
This study was approved by the Institutional Review Board of the Medical School of Wisconsin (Milwaukee, WI).
Patients were included in this study if, (1) their primary hyperhidrosis disease was diagnosed based on patient history and evapotranspiration; (2) traditional and conservative treatments do not work for them; (3) they have not performed any surgery in the armpit area for this condition; (4) surgical treatment with arthroscopic shaver technique (5) at least three months of follow-up, including the evaluation of the evaporimeter after the operation.
There were no age, gender, or ethnic criteria.
When this study started in 2005, its design was used only to examine the patient to evaluate the results and request each patient to return to the clinic in order to perform the starch and iodine test after the operation. Since the addition of the evaporimeter in April 2009, all former patients treated before the evaporimeter procedure have been asked to return to the clinic in order to review the information after the evaporimeter procedure. For subsequent patients in this series, evaporimeter data review is included in both initial and postoperative assessments to document short- and long-term outcomes.
Twenty-nine patients were being treated between March 2005 and March 2009, when the evaporimeter became available; Another eight patients were treated according to the full study protocol between April 2009 and June 2010.

Figure 3. Local anesthesia containing epinephrine is injected before preparing the axillary area.
Surgical procedure
As the affected sweat glands are related to the area with hair in the armpit, this area is shaved and marked before induction. The 1-cm access incision site, located in the anterior axillary slit, is also marked (Figure 2). The patient is placed under general anesthesia in a lying position on his back and arms at an angle of 100 degrees away from the body axis to take care and avoid the risk of damage to the nerve network.
Approximately 20 to 30 ml of 0.5% xylocaine (lidocaine) with a concentration of 1 to 200 epinephrine is given bilaterally and enough to penetrate the surface, to create a boil (Figure 3). This injection is important to stop bleeding (hemostasis) and control short-term pain after surgery. After that, the patient is prepared, so there will be enough time to maximize the effects of epinephrine.
A 1 cm incision is made in the marked area in the anterior and mid axillary region. Using Metzenbaum surgical scissors placed horizontally through the incision, the axillary hairy skin surface is kept high, leaving as little subcutaneous fat as possible in the raised flap (Figure 4).

Figure 4: Curved Metzenbaum scissors are used to raise the hairy surface of the axilla, leaving a small amount of subcutaneous tissue on the skin flap.

Figure 5. Orthopedic cartilage shaver used to remove deep skin tissue, which contains the affected sweat glands.
The operation was performed quickly and in a bloodless manner, taking care to ensure that the flap was fully raised in the marked area. A suction-assisted cartilage shaver with a Stryker CORE system equipped with a pocket-mounted controller driver device (Stryker Kalamazoo, Michigan) (Figure 5). This shaver is usually used in nerve joint surgery with endoscopic orthopedic cartilage shaver technique, including two concentric metal cannulas, one smaller than the other. At its tip, the outer, larger cannula has a semi-open section that protects the sharp, oscillating inner cannula; which allows two cannulas to provide both continuous curettage and suction evacuation, which is simultaneously active with the rotating curette (Figure 6).
The hand setting was set to 900 rpm, the lowest setting value. The tip of the shaver is always placed upwards (toward the lower surface of the raised flap) to prevent damage to deeper tissues. The best placement was obtained by applying the shaver from the head of the table, above the patient's outstretched arm. With the activation of the oscillating blade and suction, the suction of the subcutaneous tissue in the tube was clear.

Figure 6. Close-up of the semi-open cannula, which includes the oscillating blade and suction.

Figure 7. Stabilization of the axillary skin by two assistants is essential to maximize safety and efficacy.
Having an assistant to keep the axillary skin taut during the scissor lift phase and main surgery helps the Shaver method to avoid axillary skin perforation (Figure 7). This stabilization of the skin is of great importance, as it facilitates the limitation of the depth of the subcutaneous fat at the deep level of the interdermal layer (which includes the affected sweat glands), while protecting the follicular structures and related skin structures. At the stage of completing the shaver surgery, to prove the complete removal of the subcutaneous tissue and maintain the integrity of the axillary skin, the skin is turned back and forth (Figure 8).
For drainage, a soft drain with small holes was passed through the incision, the skin was closed with a simple nylon suture, and a sponge pad with silk sutures was placed in the axilla to provide external pressure (Figure 9).
24 hours later, the drain and external pad were removed in the clinic. The whole process was completed within an hour. Most patients reported little pain. Nevertheless, painkillers were prescribed.

Figure 8. The back and front of the wound at the end of the surgery shows the absence of subcutaneous tissue and the base of intact hair follicles, and as a result, it will be ensured that the affected sweat glands, which are located in the deep middle layers of the skin and under the follicles, are completely removed.
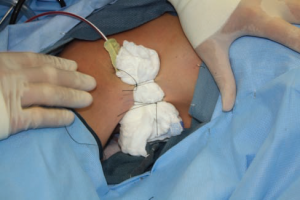
Figure 9. After placing the drain through the wound, an external dressing (sponge pad) is placed in place to eliminate dead spaces. Within 24 hours, the drain and pad are removed.
When the external dressing was removed, patients noticed that sweating stopped. After surgery, patients were asked to limit their arm movements for one week. The stitches were removed in five days. The usual absence from work after surgery was about four days. The condition of each patient was followed at intervals of three, six and 12 months. Evaporimeter information was obtained at each subsequent visit.
A video of the surgical procedure is available:
www.aestheticsurgeryjournal.com
You can also use your smartphone to scan the code on the first page of this article and directly view the video on www.YouTube.com.
Results
During the first four years when the researcher of this article performed hyperhidrosis surgery in the armpit area using the shaver method, the only tool to determine the degree of disability related to hyperhidrosis was the patient's history, which is very subjective and based on the five senses. Patients were simply asked to rate how the condition affected their lives on a scale of 1 to 10; The scale "1" is normal and "10" is unbearable. Although the 29 patients who underwent shaver axillary surgery between March 2005 and March 2009 were very happy with the results by this measure, the lack of objective documentation was problematic.
With the introduction of the evapometer in April 2009, the error and subjectivity of the measurement in previous years have been eliminated. Therefore, in this report, we only calculated the pre- and post-operative data of the patients in this last part of this series. There were a total of eight patients (16 axillary sites) for whom complete results are available. Seven of these patients were women and one of them was a man. The mean age of the patients was 22 years (range 12 to 35) and the mean follow-up period was eight months (range 3 to 12). The average preoperative measurements of evapotranspiration were 437 g/m2/h (range, 98-998 g/m2/h), the average postoperative measurements at the time of the patient's last visit in six months were 58 g/m2/h (range, 21-26 g/m2/h). Controls for all axillae measured an average of 23.7 g/m2/h, with a range of 18 to 31 g/m2/h.
Although not all were included in the study, between April 2005 and June 2010, the researcher treated a total of 45 patients with axillary shaver surgery. Complications include an infection, which is treated with antibiotics, and a postoperative hematoma, which must be drained in the operating room. No hypertrophic scarring, alopecia, or numbness is associated with this surgery. Although they initially responded well, two patients experienced recurrence of symptoms (and elevated evaporimeter measurements) after three months and 24 months, respectively; Both responded well to re-surgery.Discussion and exploration
Axillary hyperhidrosis causes significant social, occupational, emotional, financial, and psychological stress and problems for millions of people in the United States. In patients with primary (idiopathic) hyperhidrosis, the condition usually begins in puberty but can also appear in the late teens or 20s. There are often hereditary grounds. Focal axillary hyperhidrosis is particularly distressing, to the extent that young people are embarrassed by their condition and their social development may be limited. This situation also limits the color and type of clothing to dark and sleeveless. Many of these patients do not seek medical attention because they are shy and think that "I just sweat a lot". Recent studies have shown that a large number of patients with hyperhidrosis are at risk of secondary infections related to this disease.
Many primary care physicians have little knowledge of the treatment options available for treating axillary hyperhidrosis. When patients see a dermatologist, the options considered are usually non-surgical, although these offer only temporary relief. These interventions are sufficient for some (even many) patients, but there are definitely patients whose condition is messed up by topical antiperspirants or who are looking for a more permanent solution than repeated botulinum toxin injections. In these patients, direct intervention, surgery in the armpit area is appropriate.
The ideal process should eliminate the patient's problem permanently; be minimally invasive, simple and predictable;
It has the least problems and complications and scars. According to Baumgartner: "The main factor in surgery is to remove the offending sweat glands with as little traumatic damage as possible."
Based on the experience of this researcher and other researchers, Shaver surgery in the armpit area seems to be the ideal procedure. This procedure is a simple outpatient procedure with minimal complications and complications and provides long-lasting results due to the inactivation/removal of the sweat glands. This surgery is covered by some medical insurance in some countries. Other techniques such as liposuction have limited effectiveness and have the ability to potentially damage the structures of the armpits by using a suction cannula.
In previous reports, objective documentation of axillary sweating was limited to a tedious measurement of the weight of sweat produced or a subjective and roughly impurity measure of color change in the starch and iodine test. The results were evaluated based on mental and sensory examinations of the patient. The data presented in this objective report document vary based on the output and measurements of the evaporimeter, which measures the relative humidity in g/m2/h of the axillary area by producing highly accurate and repeatable data, allowing the adjacent hairless skin area to serve as a control area for comparison.
The pathological information of hyperhidrosis will usually be 5, 10 or 20 times more than the control area. This reassures patients that their condition is correct, while providing clinicians (and medical insurers) with objective evidence of a justifiable disease process before surgery and success after surgery. The results of this research confirm that underarm shaver surgery for hyperhidrosis or severe underarm sweating can be a simple, safe, efficient, effective and reliable outpatient procedure with minimal complications and problems, which usually reduces the amount of sweating up to ten times, and thus provides these patients with a normal state in their lives.
It should be kept in mind that the evapometer can also be used as a post-operative tool to allow doctors to evaluate patients who have undergone shaver surgery but still complain of excessive sweating. Near-normal data (generally, two or three times more than the control area) assures the patient of the effectiveness of the procedure compared to the evaporimeter data, before surgery. Of course, if the recurrence of pathological levels (10-20 times more than the control size) is recorded and proven, then objective evidence is provided to justify the repetition of the procedure
. In this review and follow-ups, resumption and recurrence of symptoms occurred in two patients (at three months and two years after surgery) after an initial excellent response to baseline.
Both patients became symptom-free after repeating Shaver's procedure, and the evapometer data also showed normal results. We don't have any more explanation for this process than what was said for the cause of initial intense sweating.
Conclusion
Until recently, the only practical way to diagnose and evaluate the results of hyperhidrosis treatment was through the patient's history in the form of pre- and post-surgery examinations, both of which showed a significant degree of subjectivity and unscientific nature. When combined with the effective surgical method of shaving or axillary curettage and suction, the evaporimeter provides an objective measurement for definitive diagnosis and confirmation of surgical results.
These documents are important in providing insurance centers with quantifiable data to justify insurance coverage and also to reassure patients who question the effectiveness of surgery. This operation also provides an essential element from the side of science for surgical intervention based on a different mentality.
As a surgeon, we should be aware of this category of patients with serious diseases that can be easily removed with a simple, minimally invasive procedure that is affordable and has predictable results so that patients can be healthy, young, happy and grateful.