Treatment of underarm sweating by the curt suction method
Surgical treatment Excessive sweating of the axilla by the sweat gland suction method
Abstract: Suction curettage is a skin surgery method to treat axillary hyperhidrosis or excessive sweating in the armpit area, which has recently become common.
Purpose: The purpose of this research is to explain the technique of removing sweat glands and evaluate its effectiveness and safety.
Result: Cort suction of sweat glands is a minimally invasive surgical technique that is easy to perform, safe, has a high success rate and relatively few side effects. In general, patients tolerate the procedures of this procedure well and compared to other surgical procedures, they need a shorter time to resume daily activities.
Key words: curtage; Suction court; hyperhidrosis; excessive underarm sweating; Lipectomy
Introduction
Hyperhidrosis or excessive underarm sweating is a common disease that has no known cause or treatment. The symptom of this disease is the secretion of sweat in excess of the normal physiological needs of the body in order to regulate the body temperature, and it can significantly affect the quality of life of the affected person. Research on quality of life shows that the negative effects of hyperhidrosis can be compared to conditions of diseases such as severe psoriasis, kidney failure, rheumatoid arthritis and multiple sclerosis. primary (idiopathic or unknown) or secondary hyperhidrosis; It is classified as general (including the whole body) or focal (local or including specific parts of the body).
Primary hyperhidrosis is idiopathic and focal. Areas of excessive sweat production are:Armpits, hands, feet and face. Affected individuals experience limitations in work, social interaction, physical activities, and leisure time. These conditions also cause mental and communication disorders for a person, which basically endangers his life. Additionally, it can lead to a variety of secondary medical conditions such as bacterial or fungal overgrowth, muscle cramps, eczematous dermatitis, among others. About two-thirds of patients have a positive family history, which indicates the possibility of a genetic predisposition.
Secondary hyperhidrosis can be both general and focal (local) and results from a latent or underlying disease such as endocrine, neurological, and infectious disorders.
Evaluation
Some of the criteria suggested for the diagnosis of primary focal (local) hyperhidrosis are: Visible, focal (local) excessive sweating for at least six months with no apparent cause, accompanied by at least two of the following features:
relatively affect the symmetrical parts of the body and bilaterally; be considered significant enough to impair daily activities; happen at least once a week; be before the age of twenty-five;
There is a family history; And focal or local sweating should be stopped during sleep.
Currently, there are several methods (mental and objective) to evaluate the amount of injury and disability caused by this disease. The Quality of Life Index with Skin Diseases (DLQI) and the Hyperhidrosis Severity Scale are two acceptable questionnaires to evaluate the impact of the disease on the patients' quality of life.
Qualitative test of starch and minor iodine and indirect iodine-starch test are two objective methods by which the amount and spread of the disease can be checked. However, tests do not provide an indication or indication of the severity of the condition or disease. To perform these tests, the armpit area must be clean, dry and hairless. In minors
In the minor starch and iodine test, the alcoholic solution of iodine is rubbed on the armpit skin. After the solution dries, the said area is covered by a thin layer of starch powder. When sweat is produced, it will come out along with two substances and produce a blue-black and purple precipitate, and thus, the test result is positive.
Verkamp and his colleagues, as well as Swin Hart, suggested the use of 3.5% alcohol iodine solution.
To perform an indirect test, pre-mix a sheet of standard A4 paper with non-powdered iodine crystals (1 gram of pure iodine per 50 sheets of paper) and store in a closed glass container for 5 days. Then we place a leaf on the axilla area for 1 minute. Hyperdrotic or perspiration disordered areas will be marked on the paper sheet with blue-violet color. In most cases, the axillary sweat glands are concentrated in a central, circular or oval area up to a size of about 4 to 5 cm. However, peripheral (external) glands may also be found. Gravimetric test, ninhydrin test and VapoMeter may be used for quantitative evaluation. However, objective methods to visualize or weigh sweat may ultimately be disappointing, as sweat rates fluctuate over time and may even stop completely at the time of medical consultation, even in untreated patients.
Although a standard definition for excessive sweating has not yet been determined, according to Cohen et al. in 2007 and Solish et al. in 2008, in practice, any type of sweating that significantly interferes with the patient's daily life (physically or psychologically, in the community or in the occupational field) should be considered as an abnormal problem. It is important to test and diagnose secondary causes (such as infectious, malignant, drug, neurological, metabolic and endocrine disorders) before diagnosing and confirming primary hyperhidrosis.
This disorder can occur at any stage of life. However, the average age at onset of the disease depends on the area involved.
The onset of underarm sweating usually occurs during adolescence.
Treatment options
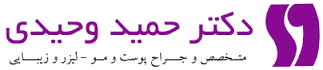
Although the medical cause of hyperhidrosis (excessive sweating) remains almost unknown, its motivational and genetic pathway
It is well known. Different treatments affect different points in this pathway, as shown in Figure 1.
Several treatment options are available to treat axillary hyperhidrosis: including topical medications, systemic medications, ionization, botulinum toxin (Botox), and various surgical procedures. Each case according to the severity and
The degree of clinical conditions as well as the advantages and disadvantages of that method should be evaluated separately. We must always remember that to treat hyperhidrosis we must always follow a step-by-step strategy using conservative methods.
Atkins et al. (2002) believe that the goal of treatment should be to reduce sweating to an acceptable level for the patient. They emphasize the importance of understanding the motivation and expectations of patients before choosing a treatment plan; Patients should be informed and advised about possible complications and limitations of all treatment options (either clinical or surgical).
Coelho and his colleagues in 2002 show that psychotherapy and psychological therapy can help, although they provide temporary relief; Therefore, it should be used for patients with extreme excitement or psychiatric and psychological diseases. A review by Massia et al (2010) showed that biofeedback and psychotherapeutic techniques have limited efficacy. According to them, these techniques require a long period of time, too much dedication and endurance from the patients, and so far only unreliable results have been obtained. However, it is important to note that although the involvement of an emotional stimulus is necessary in the creation of primary hyperhidrosis, this condition is not a mental illness but a physiological disorder.
Clinical treatment
Topical drugs are usually easily used; But they can cause skin irritation, the duration of their effect is short and in severe cases they do not have much effect. However, in most cases, topical treatment is considered as the first priority for the treatment of hyperhidrosis (excessive underarm sweating) due to its reliable and reasonable effectiveness.
Aluminum chloride is the most common agent used in this process. The recommended initial concentration is 10-15% and can be increased to 35% in ethyl alcohol (white alcohol). Although its mechanism of action is not fully understood, it is believed that it blocks the spiral duct of iontophoresis, which leads to the functional and structural degeneration of sweat glands.Iontopheresis is a method that involves the complex process of transferring ions through the skin using a galvanic current. However, this procedure is difficult to perform in the axilla area and often causes irritation. Systemic anticholinergics prevent sweating by blocking muscarinic receptors in the vicinity of eccrine sweat glands. Of course, its use is almost limited due to side effects. In any case, evidence is lacking to prove the safety and effectiveness of systemic anticholinergics for the treatment of axillary hyperhidrosis.
Because the dosage required to relieve symptoms often leads to problems and side effects such as zoosomia, palpitations, mydriasis (dilated pupils), cycloplegia, hypotension, dizziness, indigestion, and bowel dysfunction, these drugs should only be considered for acute use.
Botulinum toxin
The use of botulinum toxin is considered as a very effective and safe treatment. Fast start of activity, high level of patient satisfaction, and relatively few side effects are the advantages of this method. A dose of 1U/cm2 botulinum toxin type A (50 to 100 U per axilla) is recommended depending on the patient's response and the area and area exposed to sweating. In a study, Swartling and colleagues in 2001 measured the quality of life (DLQI) of patients treated with botulinum toxin type A. They concluded that the use of botulinum improves quality of life in patients with severe focal hyperhidrosis (excessive sweating). However, it takes 6-8 months to be effective, requires reapplication, and is expensive and not an acceptable option for many patients. Therefore, since patients usually want a permanent reduction in sweating, the benefits of this method seem limited.
Sympathectomy
Transthoracic sympathectomy surgery, which is currently preferably done through endoscopy, seems to be effective in many cases. In this method, complete or partial removal, or cutting of T3-T4 thoracic ganglia is performed to treat hyperhidrosis (excessive sweating) in the axilla region.
Unfortunately, this procedure involves many complications: complications such as arterial bleeding, intercostal vein bleeding, hemopericardium, pleural effusion (or pleural effusion) or lung adhesions, peripheral nerve damage, taste sweating, complete or mild Bernard Horner syndrome, neuralgia, hemothorax, pneumothorax, subcutaneous amysia, chylothorax, and compensatory sweating. Although most of these complications are rare, compensatory sweating is a relatively common complication after sympathectomy surgery with incidence rates ranging from 60 to 90% in some series. The areas that sweat the most are usually the back, abdomen, thighs and chest. Often, patients imagine their condition to be worse than the initial clinical picture for which they sought surgical treatment. This is the main cause of dissatisfaction in many studies. Ninety-eight percent of patients with palmar hyperhidrosis (excessive sweating) achieve complete and immediate hypohidrosis, with a low recurrence rate. However, axillary hyperhidrosis does not work as well as palmar hyperhidrosis. Therefore, currently, endoscopic transthoracic sympathectomy surgery is not the first priority treatment for focal (local) hyperhidrosis limited to the axilla. Most patients with severe localized hyperhidrosis (excessive sweating) need to consider surgery or the use of botulinum toxin as treatment options. However, since the latter option has shown significant benefits, is safer, and usually curative, Field (2003) advocates the use of botulinum for suctioning under tumescent anesthesia. The use of this poison condemns the patient to endure and pay medical expenses for a lifetime, while the curt suction is performed in a separate surgery and has reasonable expectations of treatment.
However, according to the statements of Bechara and his colleagues (2007), if the conservative treatment options are not effective, the next decision should be made with the consent of the patient and his opinion; The advantages and disadvantages of each method should be discussed without favoring one technique as the overall treatment. They point out that in these cases, doctors find themselves at a crossroads. On the one hand, they have the option of using botulinum toxin; A method that is easy and effective, but also expensive and temporary. On the other hand, there is the option of minimally invasive surgery, which requires
It takes more time and effort and has higher side effects than using botulinum toxin. However, surgery offers the potential to permanently reduce hyperhidrosis (excessive sweating), which, in this author's experience, is directly related to frequent requests from patients.
Several surgical techniques have been introduced to remove armpit sweat glands. But it was only after the emergence of minimally invasive techniques (for example, liposuction curettage, laser, liposuction with the help of ultrasonic waves, electrical surgery, cryotherapy or cold therapy, suction curettage) that its use has become more common due to its low side effects, high success rate, quick recovery of patients and leaving minimal scars. The important factor is to remove the sweat glands responsible for this situation with the least possible damage.
Minimally invasive surgical treatment
Patients are more and more demanding a safer procedure with very few side effects and complications
which will allow them to do daily activities in the shortest possible time.
The goal of local surgery for underarm hyperhidrosis is to remove the largest possible number of eccrine sweat glands in that area, and at the same time, the natural appearance of the axilla (armpit) and arm mobility should be preserved as much as possible.
Many surgical techniques have been developed and improved over the years. Baseball and his colleagues (1987) divide the most important surgical techniques into three types:
i- Methods that remove only the subcutaneous tissue without cutting and separating the skin.
ii- Complete removal of the subcutaneous tissue and covering skin
iii- Split or complete separation of the subcutaneous tissue of a small part of the central area of the axilla with the removal of the subcutaneous tissue in the adjacent areas.
However, with the emergence of new minimally invasive treatment options, Bechara et al. (2007) suggest
Type I surgery should be divided into two branches, IA and IB. The purpose of this division is to distinguish and separate the two techniques of superficial liposuction and core suction.In the first technique, only subcutaneous tissue is removed, while in the second, subcutaneous tissue and deep skin tissues are removed. There is also a difference in the effectiveness of these two techniques. Cort suction technique results in a significant decrease in sweating compared to surface liposuction. Compared to traditional surgical methods, minimally invasive techniques offer several advantages, such as reducing the risk of infection, reducing post-operative pain and shorter recovery time, and leaving minimal scars, etc. However, to perform these procedures on the small area used in surgery, it requires high skill of surgeons.
Court Suction Technique (IB – Baseball / Bechara)
Treatment of axillary hyperhidrosis through surgery and removal of sweat glands consists of removal of eccrine, apocrine and apo-eccrine glands of the deep interdermal tissue and subcutaneous cellular tissue of this area (Figure 1 and Figure 3). There are many variations of this technique.
Chart 2
Minimally invasive surgery technique
| Type IA: removal of subcutaneous tissue (SCCT) without skin removal (superficial liposuction) Type IB: removal of SCCT and deep interdermal layer without skin removal (cort suction) Type II: complete removal of subcutaneous tissue and SCCT and covering skin Type III: complete removal of a small part of the central axilla area and removal of SCCT from the adjacent area |




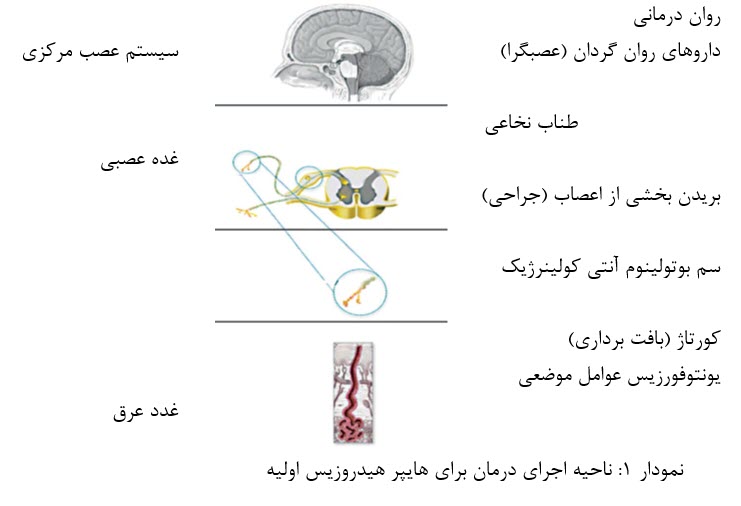
Removal of sweat glands through suction cup. Image A: Thomsent Anesthesia; Image B: Extraction of sweat glands using a curt (spoon) upwards; C and D: pressure dressing
Diagram 3: Step-by-step explanation of axillary sweat glands removal through curt suction
1. Adjusting the patient's position 2. Compliance with the principles of asepsis (disinfection) and antisepsis 3. Penetration of primary local anesthesia 4. gap 5. Preparation and placement of penetrating cannula• Thomsent anesthesia (Figure A 1)
• Back and forth movements to create subcutaneous tunnels
6. Removal of glands with the curt upwards (Figure B 1) 7. Suction (skin and subcutaneous tissue) – optional 8. Suturing 9. Pressure dressing (Figure C 1 and D 1)This method consists of two main parts: dissecting the interdermal layer in the overlying subcutaneous cellular tissue, and then harvesting the sweat glands of the deep interdermal layer and the interdermal layer/subcutaneous junction.
This procedure is currently performed on an outpatient basis and with Thomsent anesthesia.
The extent of the treatment range is generally from 1 to 2 cm beyond the hair surface. However, to determine the affected area and prevent the return of the remaining areas of hyperhidrosis, starch and iodine tests can be performed before surgery. Some authors prefer to trim axilla hair 2 to 3 days before surgery. Other authors prefer to keep them, because they facilitate visual observation and marking of the treated area during the treatment process and help as a stopping parameter. Patients are placed in a supine position and their arms are moved away from the body axis at an angle of 90 to 135 degrees so that the axilla area is exposed. To avoid damage to the brachial network, the arms should not be too far away from the body.
For surgical access, two to three small incisions are made on the outside of the area to be shaved.
These slits are created in different places according to the preference of the surgeon: from the midline view of the axilla, in the anterior and posterior edges, in the uppermost inner area of the arm and in the central part of the axilla.
Then the amount of 100-500 ml of Tumsent solution is gradually passed as superficially as possible to the pre-specified area in each axilla to leave an orange peel effect in the covering tissue.
Although the standard formulation for Thomson anesthesia is 1000 mL of normal saline solution, 50-100 mL of
Lidocaine is 1%, 1 ml epinephrine 1000:1 and 12.5 ml sodium bicarbonate, there are many other formulations used by different authors.
Volina and colleagues (2008), for example, used a solution consisting of 1000 ml of Ringer's solution, 50 ml of prillocarpine and 1 ml of 1000:1 epinephrine solution in their research. This solution reduces bleeding, makes dissection easier and reduces bruising or ecchymosis.
The long-term analgesic effect after lidocaine tissue accumulation guarantees a relatively pain-free postoperative period.
Expansion and expansion of axillary soft tissues minimizes the risk of damage to the brachial plexus. Also, as an advantage, it eliminates the risks associated with general anesthesia, the use of intravenous sedation, and analgesic and addictive drugs. Of course, it is important that the solution is prepared shortly before surgery, because adrenaline does not remain stable for long. The use of injection cannulas with a small diameter is very important for patient comfort. After whitening the desired area, in order to separate the skin of the subcutaneous tissue, subcutaneous tunnels are created by shaving, with back and forth movements. Finally, the subcutaneous sweat glands are ready to move and separate. After that, a casio cannula (or curette) is inserted for suction and skin curettage. Suction of the removed tissue can be done manually or using an instrument or device. In manual suction, a syringe is attached to the cannula, which is inserted into the tissue to be removed before the plunger is withdrawn.
Using a mechanical lock is necessary to keep the plunger open. But, this system does not have deep and continuous suction. If part of the cannula is accidentally removed during suction near the slits, the suction may be interrupted and it is considered one of the weaknesses of this method. If this happens, the air trapped in the syringe must be removed before reuse.
In the mechanical suction system, the cannula is connected to the collection bottle through a tube. The tissue removed by the cannulas is transferred into the reservoir through a collection system, using negative pressure generated by a suction pump. The size of the cannula and its opening, as well as the amount of suction performed and the speed of the cannula stroke directly affect the amount of tissue removed.
The surgeon can use his non-dominant hand to squeeze the skin in this process. Curtage around the incision site should be performed with great care and precision, because the subcutaneous tissue near the incisions may not be adequately removed by liposuction alone.
Row and his colleagues (2008) at the end of this process, the surgeon washed the wound abundantly and stopped the bleeding with great care, and then closed the surgical incisions. They recommend the use of anchoring sutures in the area treated with liposuction and aggressive curettage because it reduces the formation of hematomas or blood clots. Dressing can be done with antibiotic ointment. Some authors offer prophylactic antibiotic treatment to patients before surgery. There are reports of the use of an arthroscopic shaver to complete this procedure.
Such tools have a double cannular structure. Its internal cannula is used for rotation, and as a continuous-acting cort. The outer cannula is also used to protect the epidermis from direct damage during curettage-liposuction. If an arthroscopic shaver is used to perform this procedure, this device is placed in the armpit area after the interdermal layer and the subcutaneous cellular tissue is dissected with scissors.
Before activating the blade or suction device, tunneling is done. The shaver blade should only be turned on during the idle phase and the machine should not be passed over the same area more than once or twice. To avoid damage to deep nerves and blood vessels, the tip of the shaver should always face upwards. A suction tube is attached to the shaver handle for quick removal of shaved tissue. The number of rotations per minute for the inner cannula varies in different studies.
According to Li et al. (2005), this system should be set to oscillate to maintain rotation of the inner cannula at 1500 rpm. Wu et al. (2009) used it at 2500 rpm while Chern et al. (2010) preferred to keep it at 500 rpm.
Arenja and his colleagues set the suction device at 50 mmHg (millimeters of mercury) in their research. Larson et al. (2010) stated that in order to prevent skin perforation, an assistant physician should perform manual traction to stabilize the axillary skin both during tissue dissection with scissors and during the curtage procedure itself.
Comparative analysis of IA and IB techniques (baseball / baseball)
A study conducted by Beer and his colleagues (2006) 87 showed that the majority of all types of sweat glands (eccrine, apocrine and apo-eccrine) in the armpits of Caucasian adults are located in the subcutaneous tissue, at the boundary of the interdermal layer (not in the interdermal layer itself). These findings suggest optimization of type I surgery by avoiding more radical surgical techniques (type II and III), which have a higher infection rate and leave unpleasant scar marks. However, the authors emphasize that the success of type I surgery depends on removing sweat glands from the interdermal/subcutaneous layer interface to the point where the axillary tissue is similar to a complete skin graft.
Tisi and his colleagues (2001) conducted a study comparing liposuction and curettage techniques with liposuction for the treatment of osmidrosis. The results showed that the second technique is preferred to the liposuction technique alone. Among patients treated with liposuction,
10% were satisfied, 70% were somewhat satisfied and 20% were dissatisfied. After treatment with curettage and suction, 80% of patients were satisfied and 20% of them were somewhat satisfied.
In the research conducted by Grazer and his colleagues (1992) in order to analyze the use of liposuction for the treatment of hyperhidrosis, the recurrence rate was announced as 30%. Although this method has many advantages - such as the small size of the wounds, short recovery period, few complications and undetectable scar (scar) - some sweat glands adhere firmly to the interdermal layer and are difficult to completely remove with this type of method.
Since it requires considerable force to separate the glands from their ducts or ducts, it can be impossible to remove all the subcutaneous glands using superficial liposuction alone.
Park and Shin (2001) analyzed the histopathology of three patients and showed that when blunt cannulas are used in liposuction to shave the interdermal layer, the removal of sweat glands is not done adequately. Therefore, whenever curettage is performed, a cutting tool is essential for effective removal of sweat glands located deep in the interdermal layer.
In a study published in 2008, Bechara and his colleagues confirmed that curettage combined with liposuction is effective in removing sweat glands through pathological analysis of tissues from suctioned material during surgery. Normal or destroyed glands were found in specimens taken from all patients, and sections of connective tissue were observed in suction. This shows that this method allows not only the removal of the glands in the subcutaneous fat, but also the curettage in the interdermal layer. Tissue pathology in all biopsies of patients who were treated with this surgical method showed that the axilla surgical skin was similar to a complete skin graft. Out of a total of 15 patients who were examined with this technique, 1 (one) person showed only a slight decrease in the amount of sweating. However, since the pathological analysis of the tissues showed a large number of remaining sweat glands, the authors concluded that the procedure was not invasive enough on the subject.
The technique consisting of curettage and mechanical suction, which is performed using an arthroscopic shaver, has the advantage of faster surgery compared to manual curettage. However, inexperienced surgeons using this technique should be aware of the possibility of axillary skin perforation. If the suction is too strong, the dermis can be strongly sucked against the blade. Bechara et al. (2007) point out that compared to other techniques such as curettage, superficial liposuction and curettage-liposuction, extensive practice is necessary to avoid such things as skin perforation. These authors also emphasize the high costs of materials required in this method. From this point of view, the suction court is a significantly more favorable method in terms of cost-effectiveness and provides similar results.
In a study for the treatment of severe body odor, Lee et al (2005) reported a reduction in skin perforations using a modified external cannula. In order to protect the interdermal layer against the internal spoon, the opening of this external cannula has a grid. These authors suggest that careful manipulation of the thickness of the axillary skin is performed in order to avoid deep shaving and thus the risk of vascular damage.
canola selection
According to Bechara et al. (2007), minimally invasive surgery will provide promising results only if it is accompanied by strong resection or removal of the glands in the middle layer of the skin and make the skin tissue similar to the tissue of a complete skin graft. This area can supply the blood it needs from the surrounding skin that has not been operated on.
Therefore, when performing curettage in the depth of the interdermal layer, in order to effectively remove and harvest the sweat glands (Figure 2), cutting tools are necessary. In this figure, the use of various cannulas with a sharp surface is described: liposuction cannulas, gynecological cannulas, sharp spoons, special cannulas designed for this purpose. However, the choice of canola used among authors in this field is very diverse. In general, this choice is made based on the personal experience of the surgeon or suggestions taken from separate case reports. Fatemi cannula has a diameter of 3 mm and a length of 20 cm and has the ability to perform suction and curettage at the same time. Its ability to destroy both eccrine and apocrine glands has already been proven. However, Bechara et al. (2007) criticize the small holes on its side, which often get stuck in the skin tissue and limit an efficient curettage in the depth of the interdermal layer. In addition, the diameter of this cannula is also very small. Although the Fatemi cannula has cutting edges, it has structural limitations that prevent it from achieving sufficient pressure to reach the depth of the interdermal layer when a more invasive procedure is needed. However, this cannula can be used at the beginning of the process of dissection of the interdermal layer in the subcutaneous cellular tissue.
The Capistrano cannula is very similar to the Fatimi cannula, and also does not seem to offer the perfect mechanical properties for radical gland resection. The shaving edges of the holes are only slightly raised and the cannula is slightly sharp. Therefore, to perform a more aggressive process and thus obtain a higher degree of treatment, an abrasive or scraping cannula will be more suitable.
Cassio cannula can be useful because it has a cutting edge and a large hole for this purpose. However, you should be very careful when using these cannulas alone. Excessively aggressive use of these cannulas can lead to necrosis or dead skin tissue. For this reason, Kim and his colleagues (2008) suggest the connection between Fatemi and Cassio canola as a solution to this problem. One cannula compensates and completes the deficiencies of another cannula by improving the final result and reducing the risk of complications. Bechara and colleagues (2008), however, do not recommend the combined use of two cutting devices in a surgical procedure. The study conducted by this author was suspended due to the occurrence of complications in four patients who were treated with a combination of skin corts and a sharp abrasive cannula.This combination leads to extensive skin damage, disruption of the skin vascular network, and has no other benefit.
Bachara and his colleagues compared the use of three different cannulas in a 2006 article: a liposuction cannula with only one hole and a flat tip; The other cannula has three holes and a round tip
And the third cannula, which was specially made for curettage-liposuction, with 3 cutting holes and a sharp abrasive file between the holes. Although the use of all 3 cannulae led to a significant reduction in sweating, a greater reduction was seen in the group that was operated with a sharp cannula specially for this purpose. In addition, apparently the patients for whom this cannula was used were more satisfied.



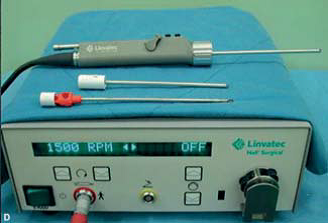
Figure 2: Instruments used for curettage
(Example): A: Fatemi cannula B: Capistrano cannula C: Recamier female curt, Casio cannula, Schroeder female curt (from left to right); D: Arthroscopic shaver
The authors attributed this success to (the fact) the special cannula that has sharp files between its holes. These files provide the possibility of aggressive shaving of the skin tissue.
Traditional liposuction cannulas may have lower efficiency due to their structure. Even cannulas with more holes are not sharp. Bechara and colleagues (2007) believe that a slightly higher rate of side effects is acceptable in the use of a more invasive cannula, because the adverse effects are not permanent or severe and most patients accept it. These authors show in this research, compared to less invasive cannulas, a wider and more invasive cannula has significantly higher effectiveness.
Interrupt the process
Because patients are more interested in a positive outcome than concerned about having focal scarring in hidden areas, Field (2003) suggests that surgeons should not hesitate to curt the target area aggressively and try to avoid few side effects or unpleasant scarring. According to this author, patients are always informed about the procedures and prefer a more invasive surgery as long as it results in a cure. However, surgeons should be aware that curettage should be performed in a manner that provides the best possible results with the least possible side effects (Figure 4 and Figure 3).
Field and colleagues (2009) reported that during curettage, the elasticity and firmness of the overlying skin is very important. Even more important is the force applied during the scraping motion, so the surgeon knows when to stop the process.
Bachara et al. (2007) suggest a number of clues and clinical guidelines for surgical procedures that indicate adequate curettage: complete lifting of the axillary skin from the subcutaneous cellular tissue; a little bruising of the axilla skin; Easy and transverse movement of the cannula under the skin (to show whether extra fat is attached to the interdermal layer or not); palpable hair follicles in the comfortable and transverse movement of the cannula under the skin; Specific sounds caused by the cannula operation due to the axilla cavity (empty space), which shows the complete separation of the interdermal layer and the subcutaneous cellular tissue.
Row and his colleagues (2008) state the symptoms of adequate curettage as follows:
Enough curettage: skin thickness (the skin becomes very thin and can be easily pinched with two fingers like a piece of clothing); Changing the color of the overlying skin (the skin becomes slightly purple, which indicates significant damage to the vascular network of the skin). According to Seo et al. (2008), at the end of this process, the skin becomes very thin and pale purple, and some dead blood spots appear. They also add another sign, that the procedure should be stopped if the following conditions occur:
Skin is sucked through the holes of the working cannula.
Chart 4: Parameters for determining adequate curation
| 1 - Thickness of the skin - the skin becomes very thin and it can be easily pinched with two fingers like a piece of clothing (Figure 3 A) 2- Skin color change - pale to purple; Dead blood stain may be seen (Figure 3 B) 3- The complete lifting of the axilla (armpit) skin from the subcutaneous cellular tissue 4- Easy and transverse movement of the subcutaneous cannula (to show whether extra fat is attached to the interdermal layer or not) 5- Palpable hair follicles in the easy and transverse movement of the subcutaneous cannula; 6- The special sounds made by the cannula 7- The skin is sucked through the holes of the working cannula (Figure 3 C) 8- The surgeon can easily remove the axillary hair by gently pulling it (Figure 3 D and E) |





Figure 3:
Parameters used for adequate curation:
A: The skin becomes very thin and easily fits between two fingers
B: The skin becomes purple and pale;
C: the skin is sucked through the suction holes of the cannula;
D and E: By gently pulling the axillary hair, the surgeon can easily remove it.
Liu et al. (2010) believe that this process should continue until the axilla hair is easily removed by the surgeon. Therefore, axilla hair must have grown to a length of 2 to 4 mm before surgery.
Wo and his colleagues (2009) in a research on the disease of strong body sweat odor (osmidrosis), provide tips to prevent necrosis or dead tissue of the skin, using arthroscopic shavers:
1) Using an internal cannula with a toothless tip, to prevent disruption and destruction of the skin or necrosis of the edges of the cracks; 2) placing a grid (grid) at the tip of the outer cannula in order to reduce skin damage; 3) It is important to keep the shaving tip active (in motion) during all procedures to prevent damage to the subcutaneous nerve network, skin destruction and necrosis of the edges of the cracks; 4) Keeping the arm away from the body axis at an angle of less than 45 degrees during the post-surgery period (21 days) reduces the stretch of the axillary skin and as a result causes poor blood circulation in the subcutaneous nerve network or edge necrosis. These authors also provide parameters for stopping the surgical procedure:
1) Direct observation under the skin with the help of two retractors. The small slits serve as a window to view possible residual apocrine glands.
2) Examination and palpation of the treated area to check the thickness of the interdermal layer.
3) confirmation of stopping the operation with the endoscopic device. This option is useful for beginners who practice estimating the desired skin thickness by touch.
Aranja and his colleagues (2007) also state that the thickness of the skin should be checked during the entire process by manual examination, and if the glandular tissue is not touched, the process should be stopped.
Other precautions
The axilla (armpit area) is an area of the body where hematoma and seroma formation is more common due to the inability to properly compress the cavity (in the axilla) created during the surgical process during the initial recovery period after the operation.
The formation of hematomas increases the risk of post-operative infection, delays healing and may lead to the formation of hypertrophic scars and disorders on the skin surface. Therefore, after the operation, large pressure dressings should be used for 2-3 days to prevent the accumulation of hematoma and seroma. Patients should be advised to avoid vigorous arm movements (especially moving the arms away from the body axis and lifting movements) for 2 weeks. Physical movement and strenuous exercise should not be done for a month. Binick and colleagues (2005) offer recommendations and recommendations for 3 weeks after surgery, local measures to prevent and improve subcutaneous fibrosis, including: local heat, massage, gel or ointment containing heparin or flavonoids. Such actions should continue for three months after surgery.
Chern and colleagues (2010) conducted a study to treat 30 patients with severe body odor (osmidrosis), in which they dissected and separated the subcutaneous tissue before liposuction-curettage. This procedure was performed through the holes opened between the fibrovascular tissues. The satisfaction rate of patients was 93%. No cases of hematoma or skin necrosis were reported. For this reason, these authors recommend careful care of subcutaneous fibrovascular bands during curettage-liposuction with an arthroscopic shaver to have a more effective clinical response and less side effects.Side effects
Although minimally invasive techniques show a relatively low complication rate, a variety of mild to moderate (mostly temporary) side effects have been reported after the procedure. Possible complications include: hematoma, ecchymosis, seroma, superficial skin erosion, loss of local sensitivity, skin necrosis, infection, hair loss, fibrosis, subcutaneous adhesions, formation of subcutaneous grafts, wounds, and recurrence of hyperhidrosis (Table 1).
Bachara and his colleagues (2007) describe the case of a patient with the rare complication of bilateral seroma. The patient had previously undergone transaxillary open breast surgery and was exposed to many adhesions that could not be separated only with a Cort suction cannula and had to be removed with scissors. These authors suggest that previous axillary surgeries should be considered as a risk factor for higher side effects. There is also a report of epidermal cysts after curettage-liposuction.
These authors believe that extensive curettage in the deep layers of the skin causes damage to the sebaceous glands of the skin and subsequent trauma or obstruction of excretory ducts. Such damage can be the main cause of alopecia (partial baldness) of the axillary skin after surgery. Rowe and colleagues (2008) suggest that trauma can be associated with abnormal repair of hair follicles, leading to structures that are unable to produce hair but produce keratin.
Final Tips
Axillary hyperhidrosis is not only considered a cosmetic problem, it is also a debilitating and uncomfortable disease.
Cort suction method is effective for treating this disorder and can significantly improve the quality of life of patients. However, it may recur after the operation.
Although the exact reason for this fact is not clearly understood and pointed out, many theories such as insufficient curettage and anatomical changes with high density of sweat glands in the upper reticular interdermal layer have been proposed.
Table 1: Side effects related to the curettage-liposuction method, related to the tools used
| Reference | Surgical method | Materials and devices used | Number of patients | Side effects (number of patients) |
| Li D. 2006 (Hyperhidrosis/osmidrosis or strong armpit odor disease) | Courtage-liposuction | Fatemi cannula | 25 (analysis of 20 people) | Temporary ecchymosis (unspecified) Local secondary infection (2) Reduction in the number of hairs (20) |
| Kim, 2008 (hyperhidrosis/smidrosis or strong armpit odor disease) | curtage-liposuction | Fatemi canola + Cassio | 65 | temporary ecchymosis (unspecified) focal alopecia (2) partial removal of smidrosis (2) recurrence Smidrosis in one year (2) Scar (scar) (1) Seroma (1) Wound opening (2) Skin peeling (2) Hyperhidrosis failure to improve (1) Axillary hyperhidrosis recurrence (1) |
| Volina, 2008 (Hyperhidrosis) | Cortage-liposuction | Canolai Fatemi Ya Sattler | 37 | mild hematoma (29) tenderness and burning around the suture (6) temporary numbness (21) minor recurrence (6) temporary subcutaneous bands, mild to moderate (4) |
| SEO, 2008 (smidrosis) | curtage- Liposuction | Fatimi cannula | 43 | Temporary ecchymosis (40) Focal necrosis of the skin (4) Skin tightening (3) Hematoma/ seroma (1) |
| Beinick, 2005 (hyperhidrosis) | Cortage-liposuction | Cannula Liposuction with a diameter of 3 to 4 mm | 15 | Hematoma (2) Recurrence of hyperhidrosis (4) Temporary fibrosis (3) Necrosis (2) |
| Bachara, 2006 (Hyperhidrosis) | Cortage-liposuction | 1. Liposuction cannula with one hole 2. Liposuction cannula with three holes 3. Sharp cannula for curettage-liposuction | 14 14 14 | Hematoma (8/6/6) Surface erosion of the skin (2/2/1) Adhesion formation (4/3/3) Seroma (1 patient in this group using a cannula with 3 holes) Burning sensation or skin (8/7/6) Partial alopecia (3/2/2) |
| Chern, 2010 (asmidrosis) | Courtage-liposuction | Arthroscopic shaver | 30 | Surgical wound infection (1 axillary area) Mild to moderate ecchymosis (28) |
| Darabanio, 2008 (hyperhidrosis) | curtage-liposuction | cannula 12 gauge | 28 | moderate surgical wound infections (4) abnormal and persistent hypertrophic scar (1) |
| Aranja, 2007 (hyperhidrosis) | Court Suction | Arthroscopic Shaver | 50 | Hypertrophic scar (1) Recurrence (3) Alopecia (1) Infection (7) Feeling of itching or burning of the skin (1) |
| Lee, 2005 (smidrosis) | Cut suction | Arthroscopic Shaver (E9005 System, Linvatec Corporation, Largo, Florida, USA) | 89 | Hypertrophic scar (1) Temporary hyperpigmentation (unspecified) Temporary hardening of the skin (unspecified) |
Continued.
Continue.
Table 1: Side effects related to the curettage -liposuction method, related to the instruments used
| Reference | Surgical method | Materials and devices used | Number of patients | Side effects (number of patients) |
| Bachara, 2008 (Hyperhidrosis) | Courtage-liposuction | Abrasive or abrasive cannula (Gaedigk GmbH, Bochum,Germany) | 15 | Hematoma (3) Skin itching or burning (4) Focal hair loss (9) Subcutaneous fibrotic adhesion (8) Seroma (1) Skin erosion (3) Necrosis (1) |
| Wu, 2009 (smidrosis) | Cort suction | Arthroscopic shaver (E9005 System, Livatec Corporation, Largo, FL) | 156 | Hematoma (2) Necrosis (10) Temporarily itching or burning sensation of the skin (5) |
| Park, 2001 (smidrosis) | Cort suction | Suction cannula with one hole | 32 | Recurrence of smidrosis (15) without side effects |
| Larson, 2011 (hyperhidrosis) | Curt Suction | Arthroscopic shaver (Stryker, Kalamazoo, Michigan) | 45 | Infection (1) Hematoma (2) Recurrence of disease symptoms (2) |
| Huang, 2010 (smidrosis) | Suction court | Arthroscopic shaver (E9005 System, Livatec Corporation, Largo, FL) | 70 | Epidermal cysts (2) Scars (5) Skin hyperpigmentation (7) New lesions due to vitiligo in the axillary region (1) |
| Bechara, 2007 (Hyperhidrosis) | Court Suction | Abrasion cannula | 51 | Echymosis (39) Skin erosion (14) Temporary adhesion formation (11) Seroma (7) Skin tingling or murmur (6) Focal hair loss (4) |
| Seo, 2008 (Esmidrosis) | Court Suction | Fatimi cannula | 43 | Temporary ecchymosis (40) Focal skin necrosis (4) Skin induration (3) Hematoma or seroma (1) |
| Bachara, 2007 (hyperhidrosis) | Cut suction (secondary surgery) | Sharp cannula Abrasion (Gaedigk GmbH, Bochum, Germany) | 19 | Superficial erosion of the skin (6) Temporary itching or burning sensation of the skin (4) Seroma (2) Temporary adhesion (6) Partial alopecia (3) |
| Rezaei, 2009 (hyperhidrosis) | Cort suction | cannula 7 mm | 168 | Seroma (5) blister-like scaling in the central area of the axilla (25) |
Other hypotheses include: compensatory disorders of the remaining sweat glands, and curettage performed in the wrong anatomical tissue layer. Findings from an endoscopic research shortly after curettage-suction by Bechara and his colleagues (2006) show that the implementation of this method at a very superficial level practically makes the complete removal of sweat glands impossible.
The findings of Lawrence and his colleagues (2006) also confirm this fact and show the presence of sweat glands in the lower part of the skin. On average, 3 to 5 mm of its thickness was determined to be occupied by glandular tissue. Bechara and his colleagues (2009) investigated the recurrence of sweating after minimally invasive procedures (liposuction and curettage-liposuction) in 24 patients using starch and iodine tests.These authors discovered three patterns of recurrence as circular, crescent and point at the site of surgical incisions. These patterns show that surgeons mainly focus on the central area of the axilla, which has the highest amount of hyperhidrotic sweating.
Table 2: Results of the curettage-liposuction method
| Reference | Number of patients | Monthly follow-up (average) | Results |
| Lee, 2006 (hyperhidrosis/osmidrosis) | 25 | 10.7 | 98% good to excellent in relation to smell 100% of patients with hyperhidrosis (3) with excellent results |
| SEO, 2008 (Esmidrosis) | 43 | 15.8 | 72.1% Good to Excellent |
| Boney, 2006 (Hyperhidrosis) | 63 | 24 | -49 patients were satisfied – 11 moderately satisfied – 3 patients were dissatisfied |
| Tsai, 2001 (asmidrosis) | 10 | not mentioned | 80% of patients were satisfied 20% were moderately satisfied |
| Chern, 2010 (Esmidrosis) | 30 | 10 | 93% good to excellent 7% acceptable results |
| Volina, 2008 (Hyperhidrosis) | 37 | 48 | 83.8% of patients were satisfied 5.4% of patients were moderately satisfied 10.8% of patients were dissatisfied |
| Aranja, 2007 (hyperhidrosis) | 50 | 28 | 96% of patients were satisfied – 2 patients were dissatisfied (due to the recurrence of the infection after the operation, not due to the recurrence of the disease itself) – in 3 patients a mild recurrence of the disease was observed |
| Lee, 2005 (asmidrosis) | 89 | 20 | Excellent results in 55 patients (61.8%) Good results in 27 patients (30.4%) Acceptable results in 7 patients (7.9%) |
| Wu, 2009 (Smidrosis) | 156 | 16 | 97.4% were satisfied – 144 patients were satisfied – 8 patients were relatively satisfied – 4 patients were dissatisfied |
| Bachara, 2007 (Hyperhidrosis) | 51 | 9 | 96.1% of patients were satisfied |
| Huang, 2010 (Esmidrosis) | 70 | 18.3 | – 24 patients were very satisfied – 41 patients were completely satisfied – 5 patients were satisfied |
| Bachara, 2007 (hyperhidrosis) | 19 | 8 | – 16 patients were completely satisfied or satisfied (84%) – 2 patients were moderately satisfied (11%) – 1 patient was not satisfied (5%) |
| Darabanio, 2008 (hyperhidrosis) | 28 | 12 | patients considered the surgical results as follows: – satisfactory 24% – good 14.3% – excellent 25% – unfavorable 39.3% |
Crescent type is always observed from the side view of the pectoral muscle and it indicates that a precise curettage has been performed in the cup depression between this muscle and the axilla. These areas around the fissures are not easily accessible with curtsy performed in the form of fan movements. And this action fuels the resistance and continuation of excessive sweating in these areas. The pressure required to shave around the cannula placement points is not enough.
Considering these findings, the authors suggest a preoperative practice that consists of marking the hyperhidrotic area through starch and iodine testing, and then performing a precise surgery on all identified sweating points.
Small areas of sweat recurrence can generally be identified by starch and iodine test. In these cases, the restricted areas can be easily removed avoiding the minimally invasive secondary method through primary ligation. Nevertheless, Bechara and his colleagues (2007) showed in a research that curettage-liposuction can be repeated in one patient, with effective results and no increase in the occurrence of serious complications.
Bachara and his colleagues (2008) conducted a study in which they evaluated blood flow in the axilla area in patients undergoing liposuction-curtage. Patients were examined before surgery and on days 1, 7 and 28 after surgery. Measurements were taken in the central area; In the area that is located two centimeters from the center of the axilla but inside the curtage area, and in the normal skin around it, it remains through the images taken with the Doppler laser. On postoperative days 1 and 7, the central area and the area 2 cm from the center had a significantly lower amount of perfusion, while the adjacent area showed a higher amount of perfusion. This fact can be consistent with the clinical observation that skin necrosis always occurs in the central axillary region. On the 28th postoperative day, no region showed significantly different values from preoperative values, although the central region still had a slight decrease in perfusion.
Cridden et al (2004) point out that there is no clear distinction between physiological sweating and pathological hyperhidrosis. Understanding hyperhyperhidrosis is highly individualized, according to these authors. In a study conducted in 2008, Darabaniu and his colleagues concluded that patients with low sweating do not benefit clinically or psychologically from the suction cup.
Therefore, these authors recommend that patients with a sweating rate higher than 25 mg/min
be selected in the gravimetric test. This work will prevent dissatisfaction of patients.
Verkamp and his colleagues (2010) believe that if the rate of sweating is higher than 50 mg/min, hyperhidrosis occurs.
According to Solish et al. (2008), and Hond et al. (2002), hyperhidrosis occurs when the rate of sweating is higher than 100 mg/5 minutes in men and 50 mg/5 minutes in women.
Bachara and his colleagues (2007) suggest that for scientific research, the effectiveness of surgical methods for
Treatment of axillary hyperhidrosis is evaluated with at least one objective measurement method. They believe that the gravimetric test is the best method to evaluate the success of surgery. This author reports that it is difficult to distinguish between patients in whom surgery has not been effective and those who are dissatisfied, although starch and iodine tests, and gravimetric tests are normal.
Probstel and his colleagues (2002) believe that a control interval of at least four weeks of gravimetric test performance is necessary after this surgical procedure; This is because during the first two weeks after surgery, sweating usually stops completely, and only then returns to a new individual level.Swinhart and his colleagues (2000) believe that a successful outcome occurs when patients are able to control their sweating using conventional antiperspirants and deodorants, because it is impossible to remove all sweat glands.
Conclusion
Curtage - liposuction of sweat glands is a safe and easy minimally invasive surgical technique. It has a high success rate and few side effects (Tables 1 and 2). Based on the analysis of Table 1, 7.47% of patients had hematoma/seroma; 2.06% had necrosis; and 1.47% had secondary infection. The analysis of Table 2 shows that the use of this method in the treatment of axillary hyperhidrosis had a success rate of up to 82%, and when it was used to treat asmidosis, the success rate was 92%. Only satisfied patients and good to excellent results were considered successful results. In general, patients tolerate the surgery well, and compared to other surgical methods, a shorter period is needed to resume daily activities (5 to 12 days). Although type IB techniques are usually quite effective and curative, patients who are not completely satisfied with the result can be treated again using the same method. This is almost always done successfully. Mastery of the technique is very important for a safe operation in this method with minimal side effects and a low recurrence rate.Although the current results are quite satisfactory, there is always room for innovation and improvement of techniques.