Table of contents
Listen to the summary of this article in this podcast:
Sleep apnea is one of the most common breathing disorders during sleep, which is characterized by the interruption or temporary reduction of air flow. Many people experience severe snoring or interrupted breathing during sleep and do not know whether this is a simple problem or a sign of a serious disease called sleep apnea. This disorder raises many questions: what exactly is sleep apnea, what are its symptoms, is there a definitive treatment for it or can only the symptoms be controlled, knowing the answers to these questions will help patients to proceed with diagnosis and treatment with more confidence.
What is sleep apnea?
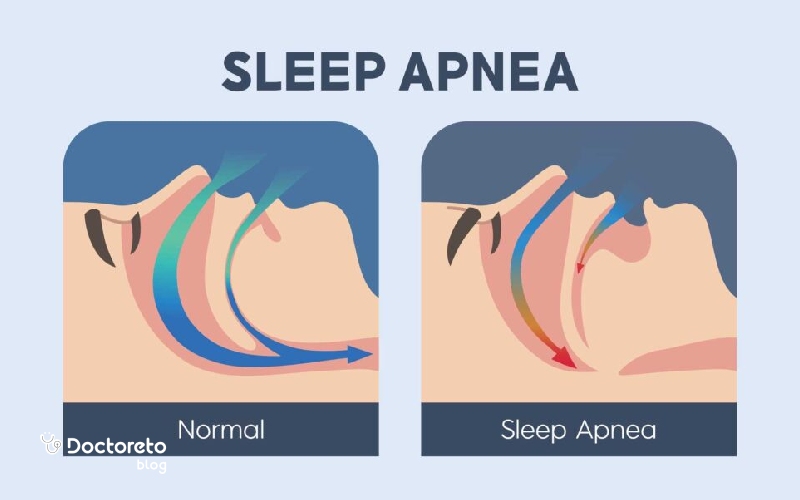
Sleep apnea is a common breathing disorder during sleep in which a person's breathing stops and starts repeatedly. These breathing stops usually last for a few seconds, but can be repeated dozens or even hundreds of times during the night. People with sleep apnea often experience frequent sleep disturbances without realizing it. This disorder is usually accompanied by symptoms such as severe snoring, sudden shortness of breath, a feeling of suffocation or coughing during sleep.
Stopping and connecting breathing causes the blood oxygen to decrease and the quality of sleep to drop drastically. As a result, the person may feel constant tiredness, sleepiness and reduced concentration the next day. If sleep apnea is not treated, it can lead to more serious consequences such as high blood pressure, heart disease and even stroke.
What are the types of sleep apnea?
Sleep apnea is not just one of sleep disorders and it can be seen in several different types depending on the cause and manner of breathing interruptions. Knowing these types is very important to choose the appropriate diagnosis and treatment method. In general, sleep apnea is classified into three main categories:
- Obstructive sleep apnea (OSA)
- Central sleep apnea (CSA)
- Mixed or complicated sleep apnea
English text:
The most common type is called obstructive sleep apnea (OSA) noopener">nhs
Obstructive Sleep Apnea (OSA)
Obstructive sleep apnea or OSA is the most common form of sleep apnea. In OSA, the muscles of the throat relax too much during sleep, causing the airway to narrow or close. This blockage prevents air from entering the lungs, even when a person is trying to breathe.
- Common symptoms: loud snoring, frequent breathing stops, feeling suffocated in sleep.
- Causes: obesity, thick neck, narrow airway (genetic), enlarged tonsils or adenoids, consumption of alcohol or sedatives, smoking, nasal congestion.
Central Sleep Apnea (CSA)
Central sleep apnea or CSA is less common and occurs due to a problem with the brain's command. In CSA, the airway is open, but the brain temporarily does not send the necessary signal to move the respiratory muscles. As a result, the person does not make any effort to breathe for a few seconds.
- Symptoms: frequent awakenings, sudden shortness of breath, superficial sleep.
- Causes: brain stem damage, heart failure, use of strong narcotic drugs (opioids), stroke.

Complex Sleep Apnea Syndrome – Mixed
Mixed apnea is a combination of obstructive and central apnea. At first, there is airway obstruction, but over time, central respiratory interruptions are also seen. It is usually diagnosed in patients who use a CPAP device to treat OSA but still have central respiratory pauses.In this video Dr. Hamed Amiri Fard neurologist talks to you about sleep apnea disorder.
What are the symptoms of sleep apnea?
Sleep apnea is not limited to snoring and can cause a range of symptoms during sleep or even during the day. These symptoms vary depending on the severity and type of sleep apnea, and in many cases, they are detected by people around the person while sleeping. The most common symptoms are:
- Loud and chronic snoring often associated with shortness of breath.
- Observable pauses in breathing during sleep, usually reported by partner or family.
- Suffocation or feeling of suffocation in sleep due to obstruction or interruption of respiratory signals.
- Waking up with dry mouth or sore throat caused by mouth breathing during the night.
- Morning headaches that occur due to lack of blood oxygen.
- Insomnia or trouble staying asleep (Insomnia).
- Excessive sleepiness during the day and constant feeling of fatigue.
- Decreased concentration and memory problems due to disturbed sleep quality.
- Mood changes such as irritability, anxiety or depression.
- Frequent need to urinate at night (Nocturia).
- Decreased libido and erectile dysfunction due to hormonal disorders and fatigue.
- Night sweats.
- Heartburn or nocturnal reflux.
- Bruxism in sleep.
- Sudden or uncontrolled weight gain, which can be both a cause and a consequence of sleep apnea.

What is the cause of sleep apnea?
Sleep apnea is usually the result of a combination of structural, genetic, and lifestyle factors that lead to blockages or disruptions in the nerve signals that control breathing. The most important causes and effective factors are:
- Obesity and overweight: the most common cause of sleep apnea. Extra tissues around the neck and throat can block the airway during sleep.
- Increase in neck size: A thicker neck is usually associated with an increased likelihood of airway obstruction.
- Congenital or genetic narrowing of the respiratory tract: some people have a narrower hereditary passage and are more prone to sleep apnea.
- Large tonsils and adenoids (especially in children): one of the main causes of sleep apnea at a young age.
- Gender: Men are more likely to suffer from sleep apnea than women, although the risk also increases in women after menopause.
- Increasing age: with increasing age, the possibility of pharyngeal muscle relaxation and apnea increases.
- Family history: Having a first-degree relative with sleep apnea increases the risk.
- Consumption of alcohol and sedatives: these substances relax the muscles of the pharynx and further block the airway.
- Smoking: inflammation and congestion of the airways caused by cigarette smoke can aggravate sleep apnea.
- Nasal congestion and allergies: Chronic nasal obstruction or allergic problems limit the normal flow of air.
- Underlying diseases: problems such as high blood pressure, heart failure, stroke or hormonal disorders (such as hypothyroidism) can increase the risk of sleep apnea.
What is the diagnosis of obstructive sleep apnea?
Sleep apnea is usually diagnosed with a combination of medical history, physical examination, and sleep tests. Doctors use the following methods to ensure the presence of sleep apnea and determine its severity:
- The doctor first examines the patient's symptoms such as severe snoring, daytime sleepiness, morning headaches and concentration problems.
- An examination of the mouth, pharynx, and nose is performed to detect airway obstruction or narrowing.
- Sleep apnea test and sleep studies are done by the doctor.
- In some cases, methods such as bronchoscopy, endoscopy or medical imaging (MRI and CT scan) are used to examine the structures of the nose, pharynx and respiratory tract more closely. These methods help to identify physical blockages or anatomical abnormalities. The severity of the disease is determined based on the apnea-hypopnea index (AHI), which indicates the number of times breathing stops or decreases per hour of sleep:
- Light: 5 to 15 events per hour
- Average: 15 to 30 events per hour
- Severe: more than 30 events per hour
Note: Apnea-Hypopnea Index (AHI) is the main criterion for determining the severity of sleep apnea. In AHI, an "Event" means a single apnea (complete cessation of airflow for at least 10 seconds) or hypopnea (a partial decrease in airflow with a drop in blood oxygen or awakening due to respiratory effort).
Sleep apnea test
Sleep studies are the main method to diagnose sleep apnea and include two types of tests: Polysomnography (PSG) and Home Sleep Test (HST).
1. Polysomnography (PSG): This test is performed in a sleep laboratory and is considered the most complete diagnostic method. In PSG, brain activity (EEG), eye movements, muscle activity, heart rate, breathing patterns, airflow, and blood oxygen levels are monitored throughout the night. In addition to diagnosing sleep apnea, this test can also detect other sleep disorders such as narcolepsy or involuntary body movements. 2. Home Sleep Test (HST): It is a simpler method that is usually used for patients with a high probability of obstructive sleep apnea. In this test, a small device at home records blood oxygen levels, heart rate, airflow, and breathing patterns. Although HST is easily performed, its accuracy and comprehensiveness is less than polysomnography.What is the treatment of sleep apnea?
The treatment of sleep apnea depends on various factors such as the severity of the disease, the type of apnea (obstructive, central or combined) and the general health status of the patient. The main goal of treatment is to prevent frequent sleep apnea, improve sleep quality, and reduce the risk of serious complications such as high blood pressure, heart disease, and stroke. According to the individual's condition, the doctor recommends one or a combination of the following methods:
- Lifestyle changes: lose weight, quit smoking, limit alcohol consumption, and develop healthy sleep habits.
- Special medical equipment: use of continuous positive airway pressure (CPAP) devices or other aids to maintain an open airway.
- Surgery: removal of excess tissue in the throat or structural modification to keep the airway open.
- Drug therapy: specific drugs in selected cases, especially in central sleep apnea.
- Traditional and herbal medicine and home remedies: complementary methods such as some medicinal plants or breathing exercises, which are recommended as adjunctive treatment and not as a substitute for standard methods.

Is the definitive treatment of sleep apnea possible with surgery?
Surgery can significantly reduce or even eliminate the symptoms of sleep apnea in some people, but it is not considered as a definitive and guaranteed treatment for all patients. Surgery for sleep apnea is usually considered when non-surgical treatments such as CPAP or oral appliances have not been successful. The choice of the type of surgery depends on the cause of the obstruction, the severity of the disease and the patient's condition:
-
Removal of excess tissue
- Includes removal of tonsils, adenoids or part of the soft palate (Uvulopalatopharyngoplasty - UPPP).
- It causes the airway to open.
- It is mostly used in people with large tonsils or blockage in the pharynx.
- There is a possibility of return of symptoms in some patients.
- With thermal energy, the excess tissue of the throat shrinks.
- A less invasive method than classical surgery.
- Suitable for mild to moderate patients or those who cannot tolerate CPAP.
- Results may require repeated sessions.
- Orthognathic surgery that moves the upper and lower jaw forward.
- It increases the airway space behind the tongue and palate.
- One of the most effective surgeries for severe cases of OSA.
- It requires a long recovery period and heavy operation.
- Implants
- Involves implanting small devices in the soft palate or tongue.
- Aim: to prevent tissue from falling or blocking during sleep.
- Some types such as pillar implants are used, but their use is limited nowadays.
- The success rate is variable.
- Tracheostomy (Tracheostomy - in severe cases)
- Creating a hole in the trachea for the direct passage of air.
- Nowadays, it is very rare and used only in very severe or treatment-resistant patients.
- Because it is invasive, it is the last treatment choice.
Bariatric surgery
- For obese patients with high BMI.
- Significant weight loss can reduce the severity of sleep apnea or even cure it.
- Sleep apnea caused by obesity usually improves significantly after surgery.
- Laser treatment (Laser treatment - NightLase)
- A non-invasive method that tightens the soft tissue of the palate with a laser.
- Aim: reduce snoring and improve air flow.
- Research is still limited and its effectiveness in treating severe OSA is not certain.
tablets for sleep apnea
Currently, there is no pill or oral medication that completely cures obstructive sleep apnea (OSA). Medications are often prescribed to manage associated symptoms such as daytime sleepiness or insomnia. For example, Modafinil or Armodafinil are used in some patients to reduce sleepiness caused by sleep apnea. In cases where the cause of apnea is related to allergies or nasal congestion, decongestants or nasal sprays can help improve breathing. However, the first line of treatment is still non-pharmacological methods such as CPAP or lifestyle changes, and drugs have only a supportive role.
Home treatment of sleep apnea
Home remedies can reduce the severity of sleep apnea, although they are not a substitute for primary treatment. Losing weight is one of the most important measures, as obesity is the main risk factor for sleep apnea. Changing your sleeping position, especially sleeping on your side instead of your back, can help keep your airway open. Avoiding alcohol, sedatives and smoking is also effective in improving symptoms. Breathing exercises and throat muscle strengthening (such as oropharyngeal exercises) have helped to reduce the severity of the disease in some studies. However, these methods are mostly effective in mild cases and are not sufficient alone in moderate to severe cases.
sleep apnea device
The most effective non-surgical treatment for sleep apnea is the use of a continuous positive airway pressure (CPAP) device. Using a mask, this device introduces a continuous flow of air into the airways and prevents them from closing while sleeping. According to studies, CPAP improves sleep quality and reduces the risk of serious complications such as high blood pressure and heart disease. Some patients use other devices, such as BiPAP or Auto-CPAP, which adjust the air pressure as needed. Although continuous use of CPAP is challenging, it remains the gold standard for sleep apnea treatment. In the table below, medical equipment that helps with sleep apnea is introduced.
| Medical Device | Description |
|---|---|
| Continuous Positive Airway Pressure (CPAP) | The most effective non-surgical treatment for moderate to severe apnea The mask provides a continuous flow of air into the airway Dramatically reduces snoring and daily sleepiness The mask may be difficult to tolerate at first be |
| Other positive pressure devices (Auto CPAP, BiPAP) | Auto CPAP: automatic adjustment of pressure based on the patient's needs BiPAP: higher pressure in inhalation and lower pressure in exhalation suitable for patients who do not tolerate CPAP or need higher pressure |
| oral devices (MRD) | a dental device that moves the lower jaw or tongue forward to prevent airway obstruction Ventilates Suitable for mild to moderate sleep apnea More comfortable and acceptable than CPAP, but less effective |
| Hypoglossal nerve stimulator | Subcutaneous device stimulates the nerve controlling the tongue Prevents tongue retraction and airway obstruction Suitable for moderate to severe patients who cannot tolerate CPAP |
| Adaptive ventilation (ASV) | Advanced device for central sleep apnea Adjusts airflow based on moment-to-moment breathing pattern Aids in balancing breathing during sleep Not recommended in some heart patients (such as heart failure with low EF) |
Treatment of sleep apnea in Islamic and traditional medicine
Islamic medicine can play a complementary role in a healthy lifestyle, but the main and standard treatment for sleep apnea is still CPAP, weight loss, surgery or medical devices. Some cases that are mentioned in the texts of Islamic medicine and hadiths and can indirectly help in reducing the symptoms:
- Weight loss: Overeating at night is prohibited and light sleep is recommended. This issue is in line with today's scientific evidence in the control of sleep apnea.
- Avoidance of alcohol and tobacco: In Islamic medicine, it is also recommended to avoid harmful substances, and this issue is one of the pillars of sleep apnea treatment in modern medicine.
- Sleeping position: It is recommended to sleep on the side instead of on the back in some narrative texts, which is in line with medical findings. Cupping and medicinal herbs: Some traditional sources mention these, but there is no strong scientific evidence that they directly affect the treatment of sleep apnea.

Is sleep apnea dangerous?
Sleep apnea is not only an annoying disorder, but if left untreated, it can have serious health consequences. Research shows that this disease increases the risk of high blood pressure, heart disease, stroke and arrhythmia. On the other hand, the resulting sleepiness and daily fatigue increase the likelihood of traffic accidents or occupational errors. In severe cases, long-term reduction in blood oxygen can even lead to sudden death. Therefore, it is necessary to see a doctor and start treatment on time to prevent these consequences.
Which doctor should we consult to treat sleep apnea?
If left untreated, sleep apnea can lead to serious heart problems, high blood pressure, and reduced quality of life. Therefore, if you see the following symptoms, you should see a doctor:- Severe and continuous snoring that disturbs the sleep of oneself or others.
- breathing interruptions in sleep that are observed by the people around.
- Excessive tiredness or sleepiness during the day that affects concentration and performance.
- Possible connection with other health problems such as heart disease, stroke or memory and concentration problems.
Timely diagnosis and treatment can prevent the occurrence of serious complications and significantly improve the quality of a person's life.