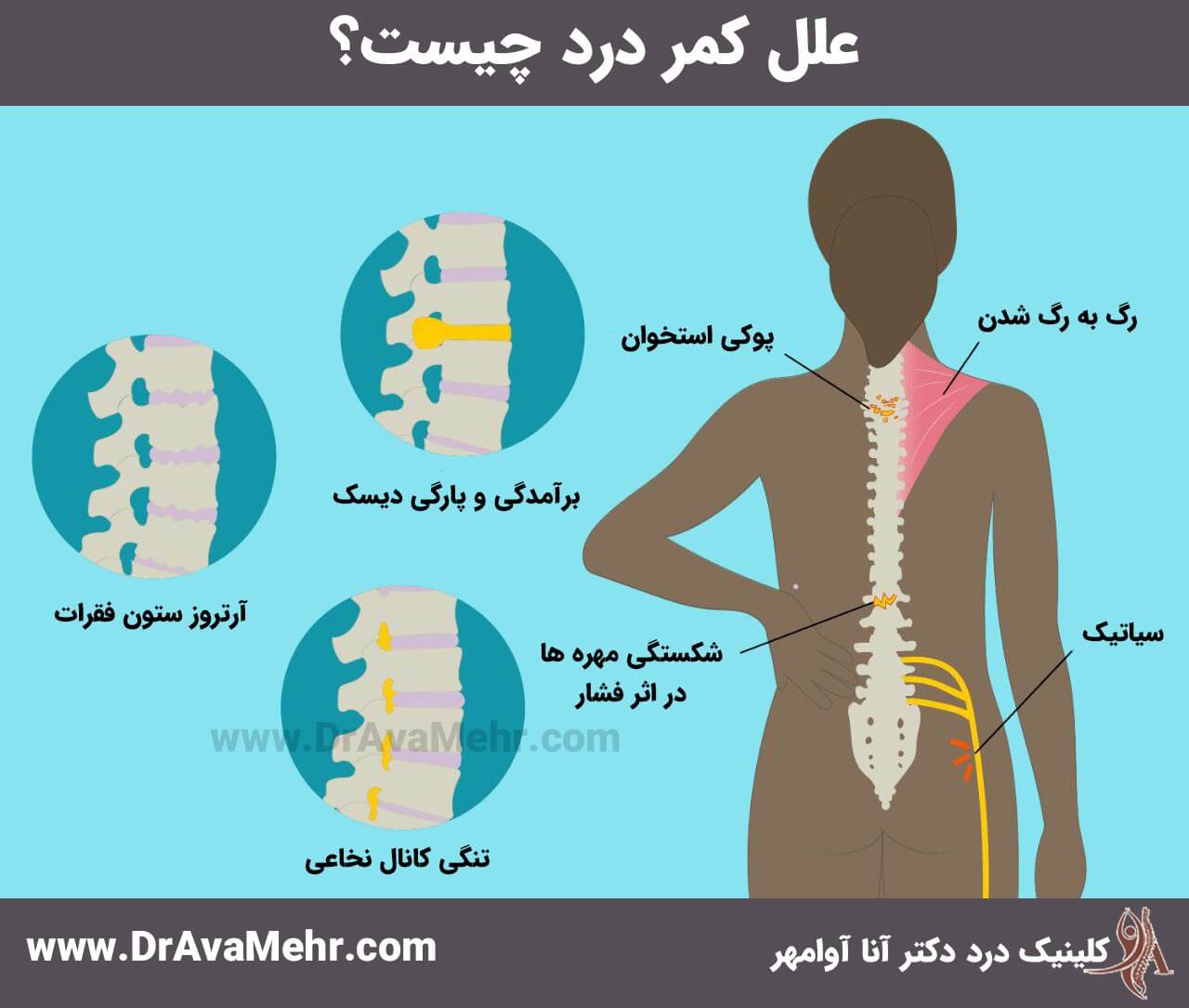
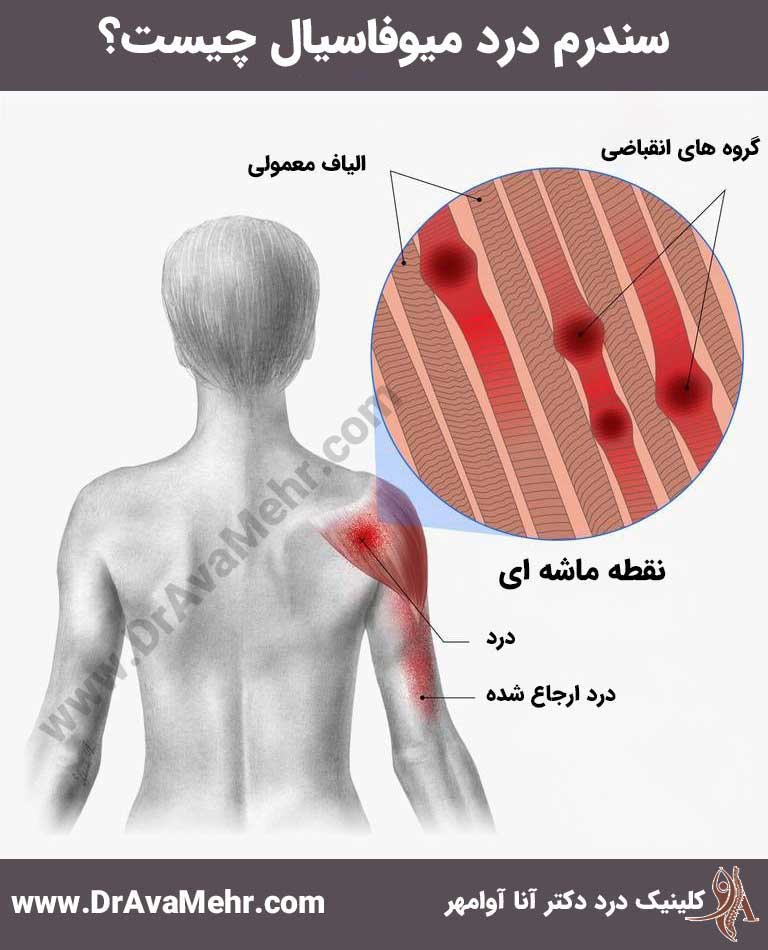
Myofascial pain syndrome is a chronic condition caused by inflammation in the muscles and fascia (the thin, connective tissue that surrounds your muscles). "Myo" means muscle and "fascial" means fascia.
If your body were an orange, your skin would be the orange peel, your muscles would be the fleshy orange, and the thin white membrane surrounding the orange would be the fascia. Fascia surrounds all levels of muscle tissue—muscle fibers, individual muscles, and muscle groups.
For most people, myofascial pain occurs in a specific area. But in some cases, it can affect multiple areas (but usually on one side of your body).
syndrome How common is myofascial pain?
Myofascial pain syndrome is very common. Experts estimate that up to 85% of the general population will be affected by this disease at some point.Symptoms and causes
What does myofascial pain syndrome feel like?
Symptoms are different for each person with myofascial pain syndrome. Sometimes the pain happens suddenly and all at once. Other times it's a constant, numbing pain, the kind that always lingers in the background.

Symptoms of myofascial pain syndrome are:
- Pain that is aching, throbbing, with stiffness, cramping, or similar to a nagging irritation.
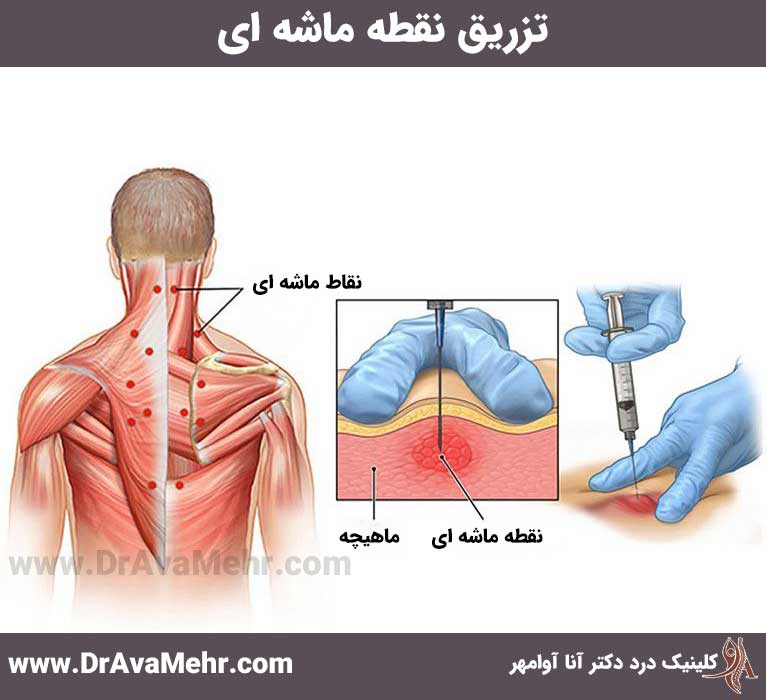
- Trigger points (small bumps, nodules, or nodules in your muscle that hurt when touched and sometimes when not touched). These areas are usually created when the condition of the syndrome worsens. Painful and sensitive muscles
- Weak muscles.
- Decreased range of motion. (For example, you may not be able to fully rotate your shoulder.)
Sometimes, people with myofascial pain syndrome also have another condition. Common problems include:
- Headache.
- Insomnia.
- Stress.
- Anxiety.
- Depression.
- Feeling tired (helplessness).
There are four types of trigger points:
- An active trigger point is usually located in each muscle. The applied pressure leads to pain in this area or along the same muscle.
- A latent trigger point is inactive, but can be activated.
- A secondary trigger point is a node in any muscle other than the muscle that has an active point. An active trigger point and a secondary trigger point can be triggered at the same time.
- A Dependent trigger point is a point that is disabled because it overlaps the area of another trigger point.
Experts are still investigating why some people are more prone to myofascial pain.
Some of the most common causes seem to be:
- Muscle injury.
- Repetitive movements (such as hammering).
- Weak physical condition.
Risk factors that may contribute to myofascial pain syndrome include:
- muscular weakness.
- lack of muscle activity (such as putting the foot in plaster).
- Working or living in a cold environment.
- Emotional stress (can cause muscle tension).
- Nerves under pressure
- Metabolic or hormonal problems such as thyroid disease or neuropathy related to diabetes.
- Vitamin deficiency, including vitamin D and folate.
- Chronic infections.
Diagnosis and myofascial pain syndrome tests
How do doctors diagnose myofascial pain syndrome?
Myofascial pain syndrome is often underdiagnosed and neglected. That's because many of its symptoms overlap with other problems that affect your nerves, bones, ligaments, or tendons.
To diagnose myofascial pain syndrome, a physical medicine specialist will need to physically examine your muscles – to feel for tight bands of muscle and then find tender points. Finding and applying pressure to a trigger point results in pain that is felt at the exact same point or in an area a short distance away (referred pain).
Are there tests that can help diagnose myofascial pain syndrome?
There is currently no test that can diagnose myofascial pain syndrome. There are also no visible symptoms such as redness, swelling, or abnormal muscle warmth.
Your doctor may recommend tests to rule out other conditions. They may also ask you questions about your symptoms, including:
- Where do you feel the pain?
- How do you describe your pain?
- How often do you experience pain?
- What makes your pain better?
- What makes your pain worse?
- Have you been injured recently?
- Do your symptoms get better at certain times of the day?
- What do you do?
- What kind of movements does your job involve?
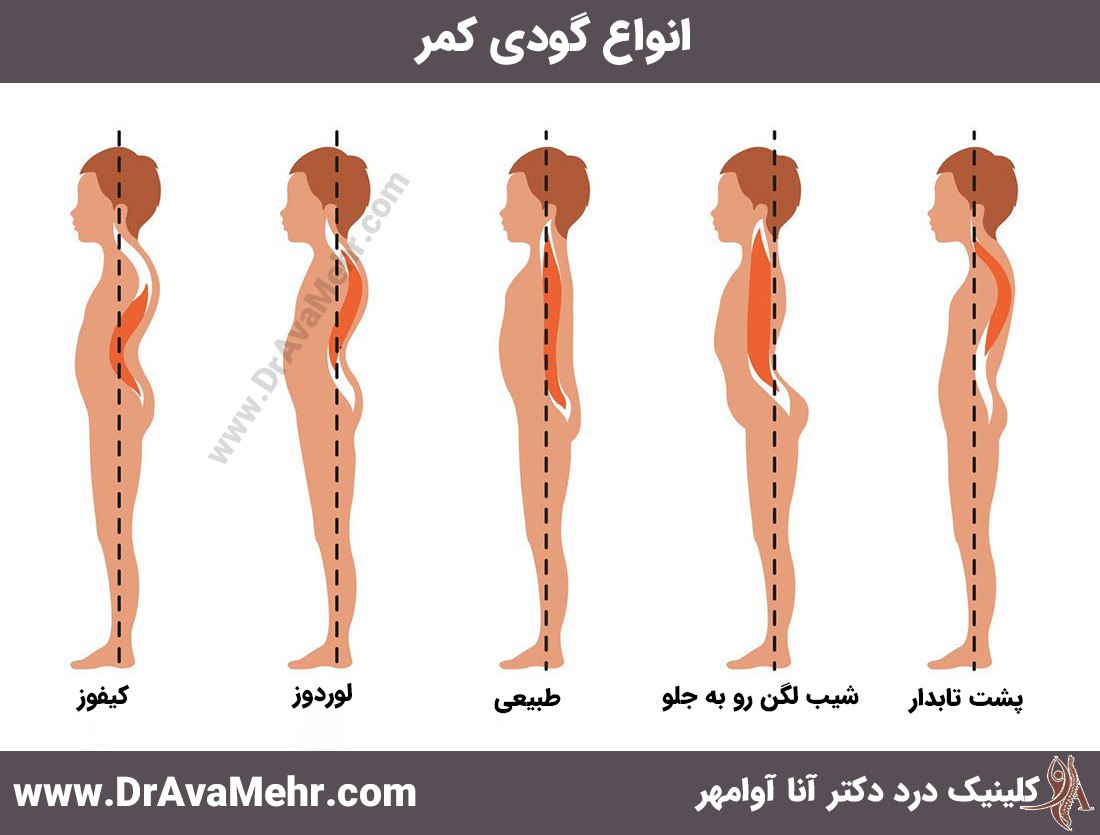
A physical therapist may check your gait (how you walk) and posture to see if there is an imbalance in muscle use and to look for signs of muscle weakness. They may also ask you about other health problems that can contribute to myofascial pain syndrome—including how much sleep you get, how well you sleep, and whether you feel stressed, anxious, or depressed.
How do doctors treat myofascial pain syndrome?
There are several treatment methods for myofascial pain syndrome, which include the following:
- In-office treatments.
- Drug.
- Home remedies.
If you have symptoms of myofascial pain syndrome, it's best to see a spine specialist early – before your pain gets worse. If you start treatment before trigger points are formed, you will recover faster.
In-office treatments for myofascial pain syndrome
The doctor will probably recommend a combination of these treatments:
- Physiotherapy to strengthen, stretch and relax muscles.
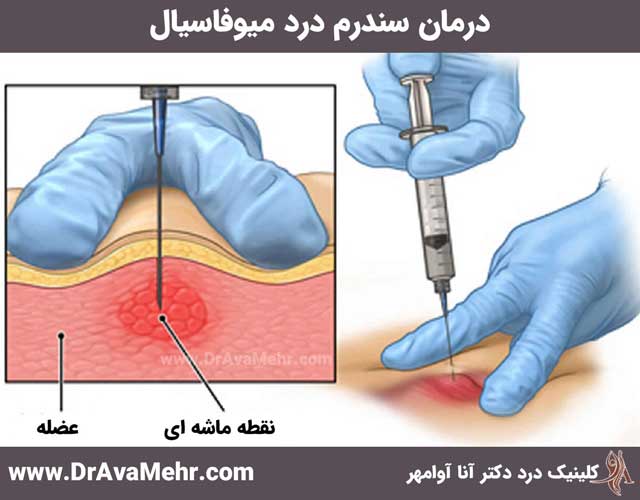
- Acupuncture (pressing thin needles into the trigger point to reduce stiffness, increase blood flow and relieve pain).
- trigger point injection (using a needle to inject lidocaine, or another anesthetic, into the trigger point to relieve pain).
- “Spray and stretch” (spraying cooling fluid on the trigger point, then gently pulling the muscles by hand).
- Low-level light therapy/cooling laser (using laser to stimulate the release of pain-relieving chemicals).
- Ultrasound therapy (using sound waves to penetrate muscles).
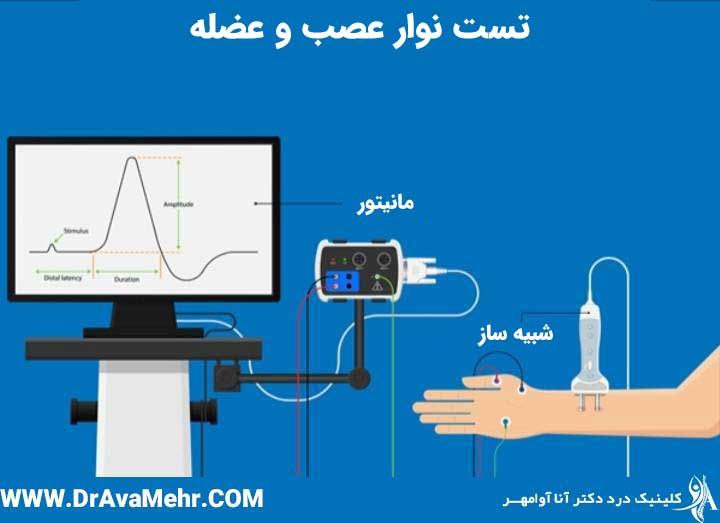
- Transcutaneous electrical nerve stimulation (TENS), where your doctor attaches pads to your skin and sends low-voltage electrical signals to trigger points.
- Acupuncture and relaxation therapies, including biofeedback and cognitive behavioral therapy (CBT) are also useful for improving sleep and reducing anxiety.
medicine
A doctor may also prescribe medications for myofascial pain syndrome, which include:
- Housing.
- Non-steroidal anti-inflammatory drugs (NSAIDs).
- Muscle relaxants.
- Steroids.
- Antidepressants.
- Sedative drugs to improve the quality of sleep.
Home Remedies
You can also try things at home to relieve your symptoms, including:
- Ice compress to reduce inflammation and thermal bags to relax muscles.
- Exercises related to myofascial pain syndrome, including weight lifting exercises (to strengthen muscles), stretching exercises (to stretch muscles), and aerobic exercises (to deliver more oxygen to muscles).
- Over-the-counter pain relievers (such as acetaminophen) or NSAIDs (such as ibuprofen or naproxen). Do not take these medications if you are using prescription pain relievers or NSAIDs.
- Relaxation techniques, including yoga (to stretch and relax muscles and reduce stress), breathing exercises and meditation.
- Dietary changes, especially avoiding foods that cause inflammation.
- Hot bath.
- Massage.
What kind of doctors treat myofascial pain syndrome?
There are several types of doctors who can treat myofascial pain syndrome, including:
- Physical medicine doctors (doctors specializing in physical medicine and rehabilitation).
- Pain management specialists.
- Rheumatologists.
- Orthopedics.
- Physiotherapists.
Can I prevent myofascial pain syndrome?
You cannot always prevent myofascial pain syndrome. But there are certain things you can do to reduce the risk:
- Observe sleep hygiene.
- Reduce your stress.
- Exercise.
- Avoid preventable muscle damage. (For example, is your bag or backpack too heavy and straining your shoulder muscles?)
- Practice relaxation techniques.
- Use a balanced diet such as the Mediterranean diet.
- Drink enough water.
mode Food for myofascial pain syndrome
Some foods cause inflammation and inflammation increases myofascial pain. Some of the foods you should avoid are:
- Fried foods (for example, French fries).
- Dairy products (milk, cheese, yogurt).
- Refined carbohydrates and foods with refined flour (pastry, white bread, pasta, breakfast cereals, pizza).
- Margarine, butter, vegetable oil.
- Sweet foods and drinks such as soft drinks.
- Red meat (burger, steak).
- Artificial sweeteners and general additives ("no sugar added" products, zero calorie "diet" drinks, processed foods including fruit, ice cream, and candy).
- Processed meat (hot dog, sausage).
Check your cupboard and refrigerator. Remove them from any foods that aggravate your myofascial pain syndrome symptoms. It's okay if you can't do it all at once. Try to eliminate one type of food at a time and go at a pace that is comfortable for you.
How can I take care of myself?
Living with myofascial pain syndrome is annoying at best and unbearable at worst. Take care of yourself by following your doctor's treatment plan and using home remedies. Try things like exercise, changing your diet, soaking in hot water, massage, etc. You may need to experiment to find out what methods work best for your pain relief.
When should I see my doctor?
If you have pain in a certain area that does not go away, see a doctor. (preferably before creating trigger points). Your doctor can run tests to rule out other conditions and come up with a plan that's right for you.
What questions should I ask my doctor?
Here are some questions you may want to ask your doctor during your appointment:
- What medications will help my myofascial pain syndrome?
- How did I get myofascial pain syndrome?
- Am I at risk for other pain problems?
- What is my treatment plan?
- Should I see a pain management specialist?
- What can I do to feel better?
- When should I come back to see you again?
Frequently asked questions
What should I expect if I have myofascial pain syndrome?
Each person's pain - including its location and intensity - is unique. The pain can flare up from time to time or be persistent and long-lasting. Successful treatment usually requires seeing a doctor you are comfortable with and following their management plan.
How long does myofascial pain syndrome last?
The duration of myofascial pain syndrome varies from person to person. With treatment, it may go away after a day or a few weeks, but it may take longer for some.
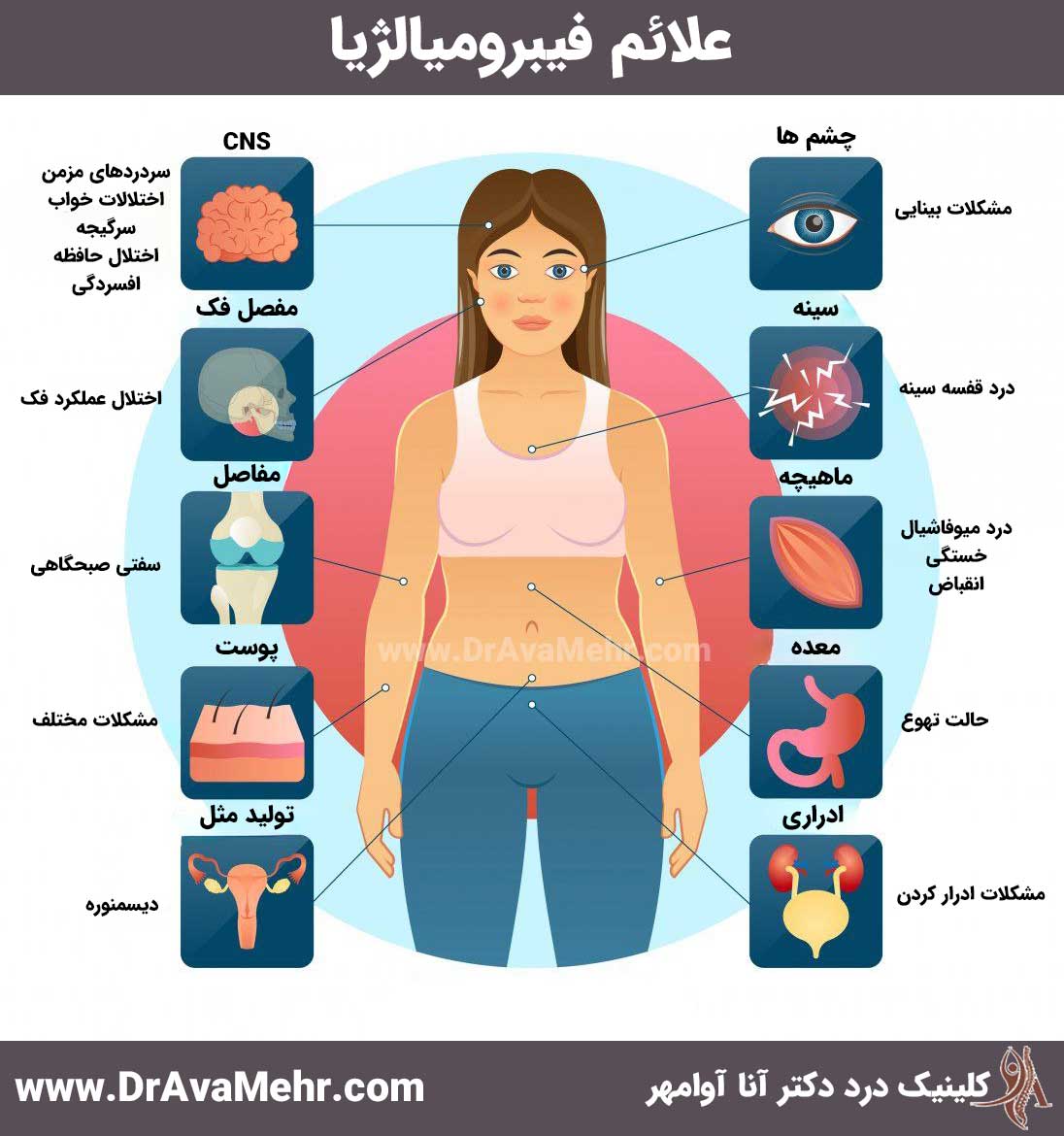
Myofascial pain syndrome vs. fibromyalgia: what's the difference?
Myofascial pain and fibromyalgia pain are similar. Both have trigger points that cause pain. But these conditions are different.While myofascial pain occurs in a specific area (or if more than one area, those areas are usually on the same side of the body), fibromyalgia pain is felt throughout the body. People with fibromyalgia mostly have the following symptoms:
- More trigger points.
- General pain.
- More severe fatigue.
- Sleep disorders.
- Headache.
- Irritable bowel syndrome (IBS).
- Additional sensations such as body swelling, burning, tingling or numbness.