Colon cancer - Dr. Karamati, colorectal surgery specialist

Dr. Mohammadreza Karamati
تهرانColorectal surgery fellowship
colon cancer
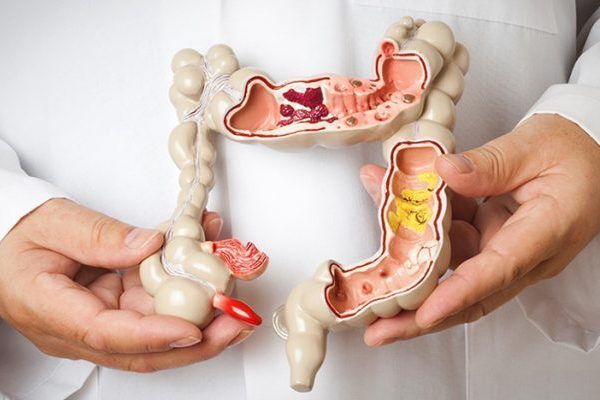
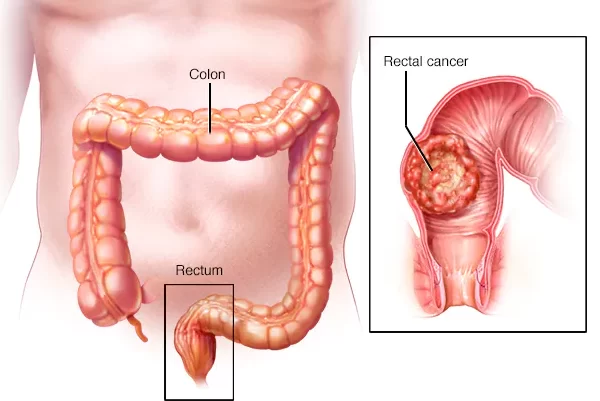
Colon cancer is a type of cancer that originates from the colon. The large intestine or colon is a part of the digestive system that is located between the small intestine and the rectum.In general, colon cancer starts when healthy colon cells undergo changes (mutations) in their cellular structure. Healthy cells grow and divide regularly to keep your body functioning normally. But when the genetic and molecular structures of a cell in the colon are damaged, they continue to divide uncontrollably even when they don't need new cells. With the accumulation of these cells, a tumor or cancer is created.
Colon tumors first appear as very small lesions or even as small and non-cancerous (benign) polyps in the large intestine. Over time and if not diagnosed or followed up in the early stages, these lesions and polyps gradually grow and can turn into cancer. These polyps and primary lesions may be asymptomatic.
Over time, cancer cells can grow and invade and destroy the surrounding normal tissue. Cancer cells can spread through the blood or lymph tissues to other parts of the body and cause metastasis.
Tumor or colon cancer can occur at any age, but its prevalence is usually higher in middle-aged and elderly people. Some people may get this type of cancer at a young age due to genetic or family predisposition.
Symptoms of colon cancer
Many people with colon cancer do not have any symptoms in the early stages of the disease or have non-specific symptoms such as weakness or fatigue. As the tumor grows, depending on its size and location in your large intestine, different symptoms are created.
Common symptoms of colon cancer are:
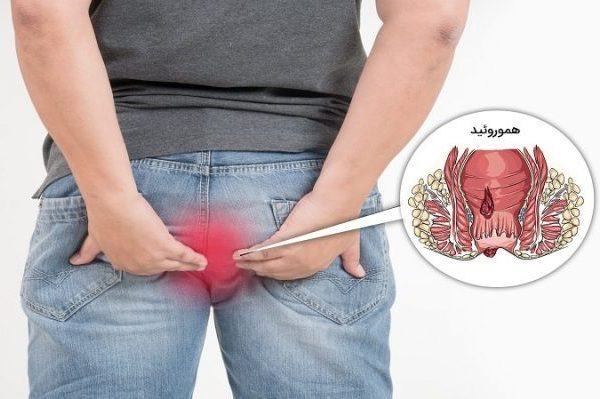
- Bleeding during defecation or seeing blood in stool
- Recent change in bowel habits (for example, diarrhea or constipation that has recently developed)
- Anemia of unknown cause
- Change in shape or consistency of stool
- Chronic abdominal pains
- Abdominal bloating that has not been treated with conventional treatments
- Unexplained weight loss
- Weakness or tiredness for no reason
Colon Cancer Screening
Regular screenings are recommended for all people to prevent colon cancer by identifying and removing small initial lesions before they become cancerous. Screening has been shown to reduce the risk of death from bowel cancer.
Guidelines generally recommend that colon cancer screening begin at age 45. But people who have risk symptoms such as bleeding in the stool or who are at higher risk, should start screening earlier and do this screening with less intervals.
There are different methods for colon cancer screening. These methods include examination of occult blood in stool, rectosigmoidoscopy and colonoscopy. If there is occult blood in the stool test, it will be necessary to perform a colonoscopy.
For more information, refer to the relevant article in the "Colorectal Cancer Screening" section.
risk factors for colon cancer
- old age
- Intestinal cancer can occur at any age, but its prevalence is usually higher in middle-aged and elderly people. The rate of colon cancer in young people is also increasing, but doctors are not sure why.
- Family history of colon cancer
- If you have a first-degree relative with this disease, you are more likely to get this cancer. If more than one member of your family has colon cancer or rectal cancer, this risk increases.
- History of cancers related to colon cancer
- If you or your first-degree relatives have a history of cancers such as gastrointestinal, breast, or gynecological cancers, you may be at a higher risk for colon cancer.
- History of colon polyp or polyposis
- If you have a history of polyps in your colon, you may be more susceptible to this cancer in the future. Of course, some of these polyps have nothing to do with cancer, and it depends on the type of polyp. But if you have polyposis (a large number of colon polyps), this possibility increases.
- Inflammatory colon diseases
- Chronic inflammatory diseases of the large intestine, such as ulcerative colitis (ulcerative colitis) or Crohn's disease, can increase the risk of developing this cancer over time.
- Hereditary and family syndromes (such as Lynch syndrome and...)
- low-fiber, high-fat diet
- Sedentary lifestyle
- Diabetes
- Alcohol
- History of radiation therapy to the abdomen for the treatment of previous cancers
- Obesity
- cigarette
diagnosis of colon cancer
Certain diagnosis of this disease is by colonoscopy and sampling. If during colonoscopy, your doctor or surgeon encounters a suspicious lesion or polyp in your colon, he will take a sample from it. Then he sends the tissue sample for pathology examination. In response to the pathology, the diagnosis of colon cancer is confirmed.
After the definitive diagnosis, a series of procedures including blood tests and imaging are requested for the patient to check the spread of the tumor in the body.
treatment of colon cancer
Treatment for colon cancer usually involves surgery to remove the cancer. Other treatments such as radiation therapy and chemotherapy may also be recommended before or after surgery.
If your tumor is early, localized, small, and completely at the tip of a polyp, your doctor may be able to remove it completely during a colonoscopy. In some of these cases, removing that polyp can lead to your complete treatment.
In cases where the colon cancer has grown but is still confined to the intestine and has not spread to other parts of the body, a colorectal surgeon can completely treat the cancer by removing part of your colon. This operation is called "colectomy" and the surgeon removes the part of your large intestine that contains cancer along with a margin of normal tissue on both sides of the cancer. Your surgeon is often able to reattach the remaining healthy parts of the colon. Nearby lymph nodes are also usually removed during bowel cancer surgery and tested for cancer. This procedure can be performed minimally invasively or laparoscopically. These surgeries are performed by colorectal surgeons.
Of course, when it is not possible to reconnect the healthy parts of the large intestine, you may need a "stoma". A stoma is a hole in the abdominal wall through which a part of the remaining intestine is removed for defecation. For easier cleaning, a bag is placed over its opening. Of course, in cases such as complete intestinal obstruction (intestinal closure) or severe bleeding, you may have to undergo emergency surgery and ostomy (bag) installation.
After the surgery and full recovery, based on your disease and the pathology (histology) result of the surgery, you may be recommended to do additional chemotherapy.
If the cancer is very advanced and unresectable or in cases where the cancer has spread to other parts of the body and cannot be removed, the doctor may not recommend surgery for the patient and chemotherapy may be recommended for the patient.
There is a possibility of disease recurrence after surgery and treatment. For this reason, after the surgery, you should be under the supervision of your colorectal surgeon frequently and at regular intervals and be sure to perform the recommended tests.
Thanks to today's modern and precise surgical methods, radiotherapy and new chemotherapy drugs, the treatment of colon cancer patients Great progress has been made. And even in many cases their disease is completely cured.
Related words:
colon cancer - colon cancer treatment - colon cancer treatment - colon surgeon - colorectal surgeon