Table of Contents
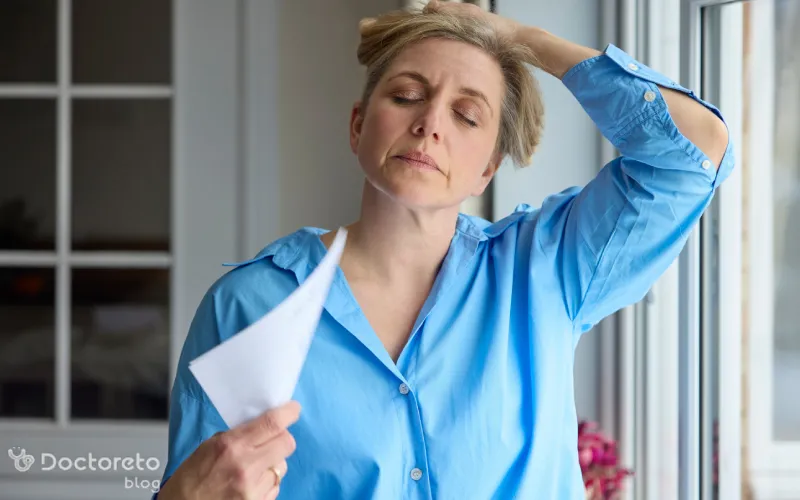
Which drugs are prescribed for menopausal hot flashes?
The best way to relieve menopausal hot flashes is to take estrogen. However, hormone use is associated with risks. If estrogen is right for you and you start within 10 years of your last period or before age 60, the benefits usually outweigh the risks. Other medications, such as some antidepressants and anticonvulsants, may also reduce hot flashes, but they are not as effective as hormones.
Discuss the pros and cons of each treatment with your specialist. If your hot flashes are not too bothersome, you probably don't need treatment; Because for most people, the symptoms will gradually decrease without treatment. However, it may take several years for the symptoms to stop completely.
| Hormonal drugs | Non-hormonal drugs |
|---|---|
| Estrogen: the most effective treatment to reduce hot flashes; Strongest effect than all options | Antidepressants (SSRI/SNRI): reduce hot flashes with less effectiveness than hormones |
| Estrogen + progesterone: effective and necessary for those with a uterus; Reducing hot flashes by protecting the endometrium | Gabapentin: reducing the intensity and frequency of hot flashes |
| Badoxifene + conjugated estrogen (Duavee): reducing menopausal symptoms and protecting the endometrium and bone | Pregabalin: reducing hot flashes with a low dose and fewer side effects |
| Local hormone therapy (cream/ring/suppository) Vaginal): suitable for vaginal symptoms; Not the first choice for generalized hot flashes | Clonidine: reduces hot flashes without affecting hormones |
| Starting estrogen before age 60 or up to 10 years after menopause: benefits usually outweigh risks | Elinxantant: significantly reduces the number and severity of hot flashes and night sweats |
hormonal drugs for menopausal hot flashes
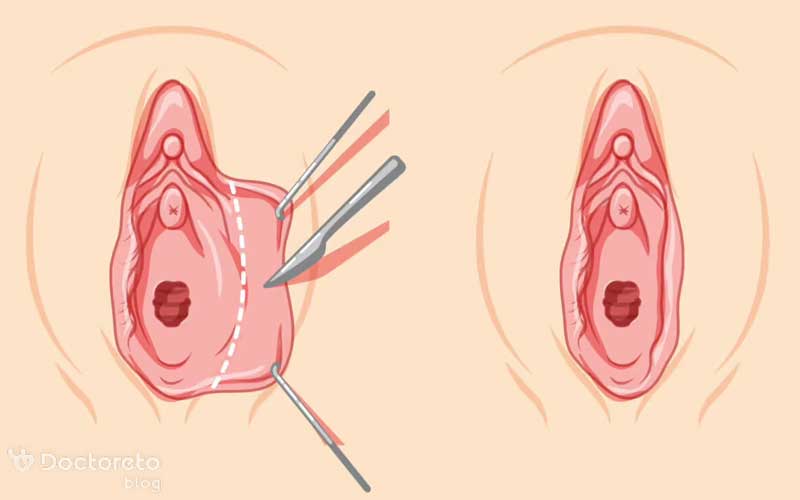
Estrogen is the main hormone prescribed to reduce hot flashes. People who have had their uterus removed (hysterectomy) usually take only estrogen. But those who still have a uterus often need to take progesterone along with estrogen. (to protect against uterine lining cancer (endometrial cancer).)
Use the lowest dose of estrogen that controls your symptoms. The duration of treatment depends on the effectiveness and potential risks. The goal is to maintain your quality of life as best as possible. Some people experience side effects when taking progesterone with estrogen. For people who cannot take progesterone, the combination drug badoxifene with conjugated estrogen (Duavee) will also reduce menopausal symptoms.
Like progesterone, this drug reduces the risk of endometrial cancer and protects bones. If you have a history of breast or endometrial cancer, heart disease, stroke, or blood clots or are at risk for these diseases, be sure to consult your doctor before starting estrogen therapy.
1. Combined estrogen and progesterone hormone therapy
In combined treatment, both estrogen and progesterone are prescribed daily without interruption. Cyclic or sequential therapy consists of daily estrogen alone followed by progesterone plus estrogen in a 28-day pattern without interruption. The duration of each stage will be different for each patient.
2. Estrogen for menopausal hot flashes
If other treatments did not work for you or if you are limited in taking or doing them, estrogen therapy may be effective. estrogen drug is effective for your menopausal hot flashes if you are experiencing menopause or had your ovaries removed before age 45, or if your ovaries stopped working before age 40.
3. Local hormone therapy
Estrogen can be taken as a pill or as a patch, gel, vaginal cream, or slow-release suppository or ring that you insert into your vagina. If you only have vaginal menopause symptoms, estrogen in the form of a cream, pill, or low-dose vaginal ring is usually a better choice than an oral pill or skin patch.
non-hormonal medications for menopausal hot flashes
Hot flashes are one of the most common and annoying symptoms of menopause. Although hormone therapy (estrogen and progesterone) is usually the most effective treatment, it is not suitable for some people. Non-hormonal drugs are a safe and effective choice for these people. These medications include certain antidepressants (SSRIs and SNRIs), anticonvulsants such as gabapentin and pregabalin, and even blood pressure medications such as clonidine. In the following, we have explained each of these drugs in more detail.1. Antidepressants (SSRI and SNRI)
Some antidepressant medications reduce menopausal hot flashes. These drugs include selected SSRIs such as paroxetine (Paxil, Brisdelle), citalopram (Celexa), and escitalopram (Lexapro), as well as SNRIs such as venlafaxine (Effexor) and desvenlafaxine (Pristiq). Studies have shown that these drugs relieve hot flashes in middle-aged women.
English text:
quoted from bmj
The studies showed that taking a daily 120 mg tablet of elizanetant significantly reduced the number and intensity of hot flushes and night sweats over 26 to 52 weeks, which compared with a placebo. The drug is administered in capsule form to be taken orally.
Persian translation:
Studies showed that daily consumption of one 120 mg tablet of Elinzantant significantly reduces the number and intensity of hot flashes and night sweats during 26 to 52 weeks. This medicine is administered orally in the form of capsules.
2. Gabapentin and pregabalin
Low-dose pregabalin reduces the number and intensity of hot flashes and has fewer side effects than higher doses. But due to limited evidence, it is no longer recommended as a treatment option in some upstream recommendations. Gabapentin is commonly used to control epilepsy or chronic neuropathic pain; However, it has also been proven to reduce menopausal hot flashes. At higher doses, the effect of gabapentin in reducing the intensity and frequency of hot flashes is less than hormone therapy.
3. Clonidine and other blood pressure medications for hot flashes
Clonidine (Catapress) is available as 100 and 25 mcg tablets. This drug is usually used to treat high blood pressure and prevent migraine headaches. It is also a non-hormonal drug that has been shown to be effective in reducing menopausal hot flashes.
English text:
Clonidine is a prescription medicine that can help reduce hot flushes and night sweats caused by menopause. You take it as tablets 2 times a day. It does not affect hormone levels, so unlike HRT it does not increase the risk of breast cancer. Farsi translation: Clonidine is a prescription drug that helps reduce hot flashes and night sweats caused by menopause. Take it as a pill twice a day. This drug does not affect hormone levels, so unlike HRT, it does not increase the risk of breast cancer. noopener">nhs
The best time to take medicine for menopause hot flashes
Take gabapentin at the same time each day. If you have just started taking estrogen pills and still have regular periods, start taking this medicine between the first and fifth days of your period. If your periods have stopped or are irregular, or you've had a hysterectomy, starting the pill at any time is fine.
Conclusion
The best medicine for menopausal hot flashes is a medicine that can both reduce your symptoms and have the least risk and side effects. This drug can be hormonal or non-hormonal, and its selection should be done in consultation with a gynecologist and based on personal conditions. For those who cannot or do not want to take hormones, non-hormonal drugs such as some antidepressants, anticonvulsants, or clonidine are good alternatives. In any case, it is better to avoid arbitrarily taking medicine to deal with these conditions.
Your doctor takes care of your health!