پیوند قرنیه چیست و چگونه انجام میشود؟
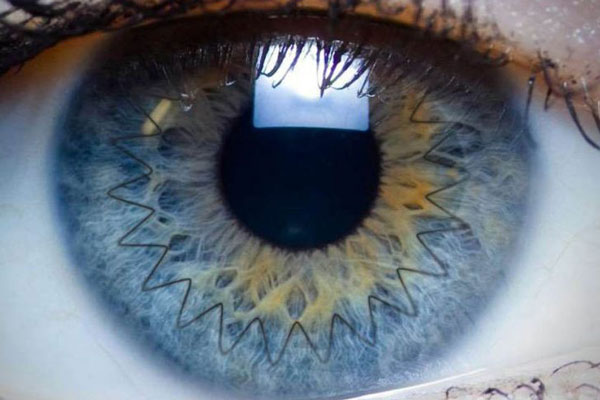
پیوند قرنیه یکی از انواع جراحیهای چشم میباشد که طی آن قرنیه اهدایی جایگزین قرنیه آسیب دیدهی بیمار میشود. دو نوع اصلی برای این پیوند وجود دارد؛ اگر کل قرنیه نیاز به جایگزینی داشته باشد، جراحی کراتوپلاستی نفوذی نامیده میشود. در صورتی که فقط بخشی از قرنیه تحت جراحی قرار گیرد، از پیوند کراتوپلاستی لایهای استفاده میشود. بافت قرنیهی اهدایی از بانک چشم تهیه میشود. عدم رسیدگی به قرنیه آسیب دیده مشکلات متعددی برای دید فرد به وجود میآورد مثلا نور به هنگام عبور از قرنیه پخش شده و از مسیر اصلی منحرف شده لذا دید فرد تار شده یا تابش خیره کنندهای را حس میکند.
در حقیقت، بیماریهای مربوط به قرنیه چشم چهارمین دلیل اساسی برای از دست دادن کامل بینایی میباشد (بعد از آب مروارید، آب سیاه و دژنراسیون ماکولا). سالانه بیش از ده میلیون نفر در جهان دچار این مشکل میشوند.
از سال ۱۹۶۱ به بعد، هر سال بیش از یک میلیون نفر با پیوند قرنیه، بهبودی بینایی خود را مجددا به دست آوردهاند.
چه زمانی نیاز به پیوند قرنیه میباشد؟
برای داشتن دیدی واضح و شفاف، وجود قرنیه سالم ضروری میباشد. اگر به دلیل بیماری یا ضربه قرنیه فرد دچار آسیب شد، به تدریج علایم بدشکلی قرنیه، درد، انحراف دید و التهاب بروز میکند.
نکته: ممکن است از پیوند قرنیه در مواردی مانند تریکيازيس نیز استفاده شود. This disease causes the eyelids to turn inward and the eyelashes to rub against the eyeball, which, if not treated, leads to wounds and eventually blindness.
This type of surgery is also recommended when medication, glasses, and contact lenses are not able to improve vision or remove painful eye inflammation.
The following items are very effective on the transparency of the cornea, and the risk of losing the cornea is very high if it occurs:
- wounds caused by infection such as eye herpes or fungal keratitis
- wounds caused by trichiasis
- hereditary diseases such as Fuchs dystrophy
- eye diseases such as advanced and severe keratoconus
- thinning of the cornea and its irregular shape (such as keratoconus)
- rare cases after surgery LASIK
- Corneal chemical burns and trauma to the eye
- Excessive swelling (edema) of the cornea
- Transplant rejection after previous transplant surgery Cornea
- Corneal loss as a result of cataract surgery
Have you met the medical conditions to receive a cornea transplant?
People who have damage and pain in the cornea as a result of an eye injury or disease, should undergo this operation to improve vision and reduce vision.
Operation time: one to two hours
Results: Significant improvement in vision
Recovery time: a few weeks to a year
Before deciding to undergo surgery, it is better to consider the following four questions:
- Does your vision have an inhibiting effect on your speech performance at work, abilities and daily activities Does it?
- Aren't other non-invasive methods such as using contact lenses able to correct your vision?
- What adverse effects does the lack of insurance cover for treatment costs from pre-operative examination to follow-ups?
- Are you able to receive a work or study leave for a period of six months to one year?
Answering these questions along with an examination and consultation with a treating physician is necessary before any action to perform this operation.
Important tips for transplant surgery Cornea
Before the cornea transplant operation
- After the final decision regarding the cornea transplant operation, the name of the patient is registered in the eye bank as an applicant for a transplant.
- The average waiting time to receive a transplant is between several days to It is a few weeks.
- Before using the transplanted tissue, the presence of any possible disease such as hepatitis and AIDS is checked based on...
- In order to maintain the safety and health of the transplant recipient, only those corneal tissues that comply with the instructions are included in the surgical process.
During the operation corneal transplant
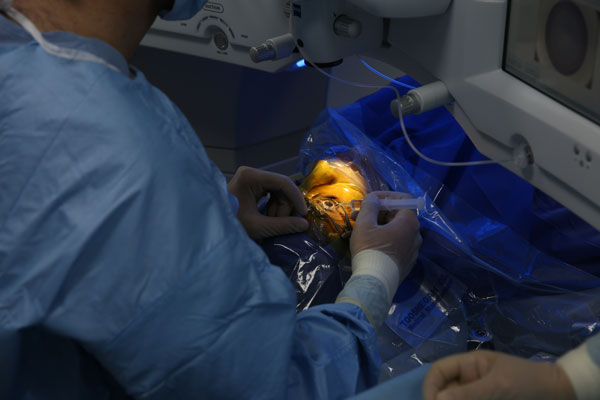
At first, the person is put under general or local anesthesia, in this case, factors such as age, health of the patient, disease or eye damage and the patient's own preference (whether he is awake or not during the operation) are considered.
For local anesthesia, an injection is first made in the skin around the eyes to gradually relax the muscles and stop eye movement and blinking for the duration of the procedure. Eye drops are also used to numb the eyes. After anesthesia, a speculum is used to keep the eyelids open. Then, the attending physician measures the area of damage in the patient's cornea to determine the amount of transplanted tissue needed.
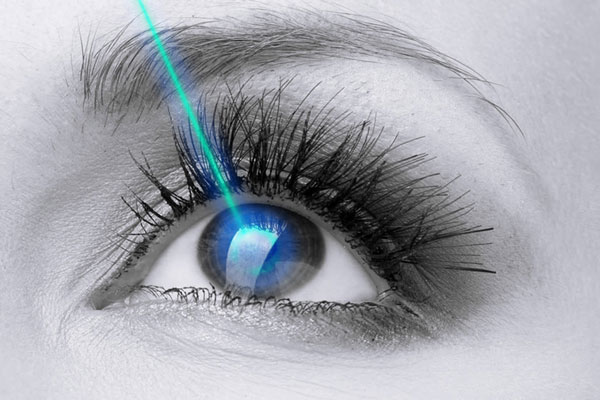
Infiltrating keratoplasty or the same common method of corneal transplant
In this procedure, a circular part in the shape of a button is removed from the full thickness of the corneal tissue by a laser or a surgical tool. Then a tissue with similar dimensions is separated from the donated cornea and placed in place to be sutured. Sutures will remain in place for a year or more. At the end, the eye is carefully bandaged. This procedure is outpatient and usually lasts between one and two hours. After that, the person is able to return home (of course, someone must take him there).
Eye tissue donation
Who is considered a cornea tissue donor?
What age is suitable for donating cornea tissue?
In the past decade, donated tissue from people over 65 years old was not accepted. Despite this, related studies have shown that tissues received from people between 34-71 years of age are completely healthy and maintain this condition for 10 years. The success rate in this situation is estimated at 75%.
Tissues obtained from young people under the age of 34 are usually used for younger people as well.
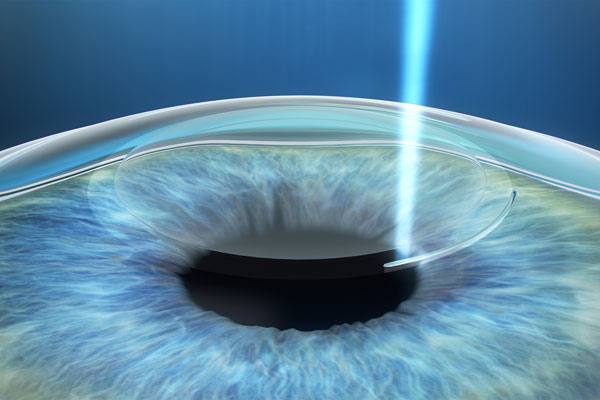
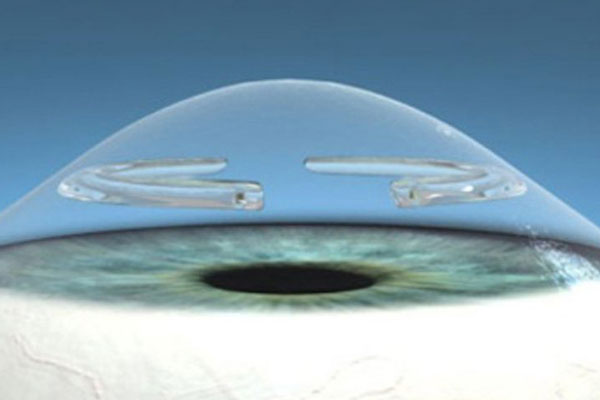
Endothelial keratoplasty
In the last decade, a new method called keratoplasty Endothelial was introduced, which can be used for certain conditions.
In this surgical procedure, the inner endothelial layer is operated on while the healthy and superficial tissue of the cornea remains intact. Epithelium is responsible for maintaining the normal fluid balance in the cornea. In case of damage to this part, there will be severe swelling that will lead to vision loss.
In this procedure, the surgeon makes a small incision to place the required tissue on the posterior surface of the cornea. This tissue is rich in healthy endothelial cells. An air bubble is used to ensure the placement of the tissue in the desired location. The incision is self-healing and there is no need to use stitches.
The newest type of it is endokeratoplasty using Desme separation method. In 2009, the American Academy of Ophthalmology announced that this operation is superior to the conventional penetrating keratoplasty method because it will result in better and more stable vision with less risks.
The endothelial keratoplasty method has advantages compared to the penetrating keratoplasty method, which are: faster vision improvement; Shorter operation time; removing a smaller amount of corneal tissue; Absence of complications caused by stitches; Less risk of astigmatism.
The endothelial keratoplasty method has become an acceptable treatment method for many endothelial disorders and Fuchs dystrophy. The penetrating keratoplasty method is usually necessary in cases where the entire corneal tissue is damaged.
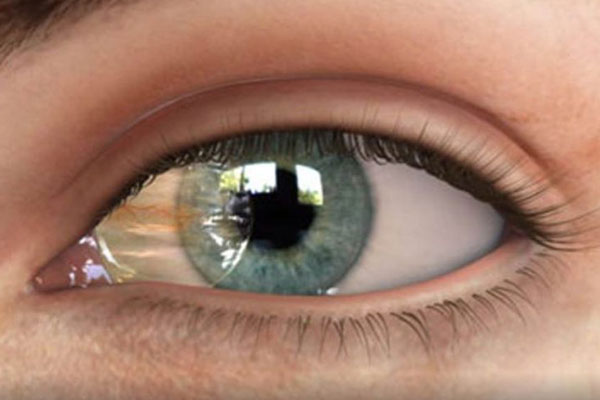
The recovery process after corneal transplant
The maximum time required for corneal transplant healing is one year or more. In the first few months after the operation, the patient has blurred vision and in In some cases, even this level of visibility is much lower than before the operation.
With the improvement of vision, the person can return to his usual activities. Of course, in the first few weeks, lifting heavy objects or performing vigorous activities is prohibited. Depending on the patient's job and vision improvement, he will be able to return to work after a week.
It is recommended to prescribe steroid eye drops for several months to allow the body to gradually accept the new tissue. To control infection, swelling and other cases, the use of special drugs is necessary. Use plastic eye protection or glasses to prevent objects from entering the eyes or damage due to impact.
If the suture is used during the transplant operation, you can go to remove it in 3 to 17 months after the operation. This important depends on the health of the eye and the healing rate of the transplant.
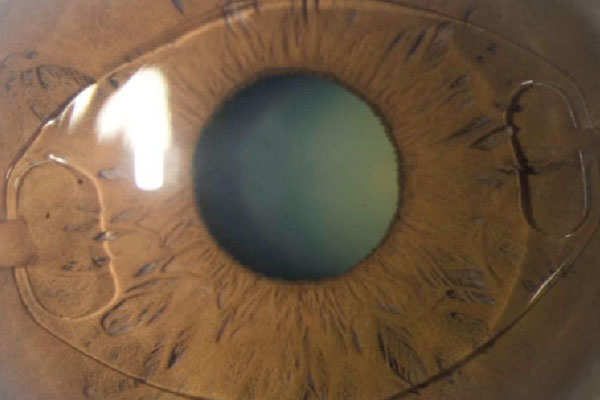
Corneal transplant rejection
Corneal transplant is very widespread and its success rate is high. In such a way that this operation has become one of the most successful organ transplant surgeries. If graft rejection is detected in time, it is often (9 out of 10) controllable and manageable.
Like any other surgery, corneal transplant is associated with possible risks. Despite this, the improvement and recovery of a person's vision after the operation is not comparable to its adverse effects.
Side effects caused by cornea transplant include graft rejection, eye infection and other issues related to the use of suture thread. Among them, graft rejection is one of the most important and occurs in 5 to 30 percent of surgeries. Transplant rejection occurs when the body's immune system perceives the new tissue as foreign and tries to eliminate it. Research shows that glaucoma and corneal swelling along with previous cataract surgery increase the chance of graft rejection.
Warning symptoms of graft rejection in its early stages are:
- Redness of the eye
- Severe sensitivity to light
- Reduced vision
- Pain
These symptoms may appear in the first month or up to several years after transplantation. These symptoms can be treated by the proper prescription of medicine by the attending physician. According to the report of the American Cornea Research Foundation, the quick identification of these signs significantly increases the success of the transplant. Of course, more time (two months to a year) is needed for this vision to become stable. After the complete healing of the cornea, the patient can use LASIK to further improve vision.
After recovery, the person suffers some refractive errors such as myopia and astigmatism, because the curvature of the new cornea is not exactly equal to the curvature of his original cornea. Therefore, refractive errors, especially astigmatism, are unavoidable. To solve these problems, it is enough to use glasses and contact lenses. Hybrid contact lenses and rigid oxygen permeable contact lenses are beneficial after transplantation. Of course, soft contact lenses can also be used.
Before going to get glasses or contact lenses, first consult your doctor to make sure that your vision is stabilized.
If you want to perform laser surgeries such as LASIK or PRK, first the eye must be completely repaired and the stitches removed from the tissue.