Perinatology (Perinatology) or Maternal-Fetal Medicine, is a specialized branch of gynecology and obstetrics that focuses on the care of
Definition of perinatology and scope of activity
According to clevelandclinic
Perinatologists, or maternal-fetal medicine specialists, are experts in high-risk pregnancies. They provide care when a medical condition, congenital disorder or disease may cause pregnancy or delivery complications.
Perinatologists or maternal and fetal medicine specialists specialize in high-risk pregnancies. They provide care when a disease, congenital disorder, or disease may cause complications during pregnancy or childbirth.
The role of the perinatologist in high-risk pregnancy care
Perinatologists play a key role in the early diagnosis and management of pathological conditions in the mother or fetus. By performing genetic screenings, specialized ultrasounds, amniocentesis and other advanced tests, they can identify congenital abnormalities, chromosomal disorders, neural tube defects or placental dysfunction.
Also, in pregnancies where the mother has a history of repeated miscarriages, premature birth or chronic medical problems, the presence of a perinatologist is necessary to reduce risks and improve pregnancy outcomes.

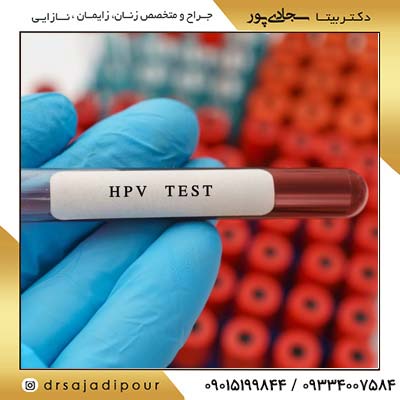
Diagnostic and therapeutic tools in perinatology
The development of imaging technologies and molecular tests in recent decades has dramatically increased the diagnostic power of this field. The following are among the most important tools used:
| Parameter | description |
| 3D and 4D specialized ultrasound | To check the anatomical structures of the fetus and diagnose congenital anomalies |
| Color Doppler | To evaluate the blood flow in fetal vessels, umbilical cord and placenta |
| amniocentesis and chorionic villus sampling (CVS) | To diagnose genetic disorders such as Down syndrome |
| maternal serum screenings | Including first and second trimester combined tests to diagnose chromosomal disorders. |
| Fetal MRI | In some special cases for a more detailed examination of the brain or internal organs of the fetus. |
About Gender determination read the above link.
Intrauterine therapeutic interventions
One of the advanced fields in perinatology is intrauterine therapy. These treatments include blood transfusions to the fetus (in cases of severe anemia), direct drug treatments, or even intrauterine surgery in certain cases such as twin-to-twin transfusion syndrome (TTTS).
Perinatology interaction with other specialties
Perinatology continuously collaborates with other medical specialties such as cardiology, endocrinology, nephrology, medical genetics, and neonatology. This collaboration plays an important role in improving clinical results, especially in the multidisciplinary care of mothers with chronic diseases or fetuses with structural abnormalities.

The role of perinatology in newborn health
One of the most important goals of this field is to reduce mortality and neonatal diseases. Perinatology interventions in preventing premature birth, controlling gestational diabetes, diagnosing fetal growth disorders and deciding on the right time for delivery have a direct impact on the survival of the baby and reducing complications in the neonatal period.
Common challenges in perinatology
Despite scientific advances, perinatology still faces challenges:
-
Diagnosis of anomalies that have no effective treatment.
-
Ethical concerns about termination of pregnancy.
-
Limited access to perinatal care in deprived areas.
-
Psychological stress of mothers facing high-risk pregnancies.

The future of perinatology; Artificial intelligence and advanced genetics
New trends in medicine such as the use of artificial intelligence for ultrasound analysis, risk modeling, and genetic analysis provide a bright future for perinatology. Also, progress in gene editing (CRISPR) and gene therapy can provide the possibility of treating some genetic diseases in the fetus.

Conclusion
Perinatology, as an interdisciplinary specialized field, plays a vital role in maintaining the health of the mother and the fetus in high-risk pregnancies. The importance of early diagnosis, careful monitoring and therapeutic interventions in reducing infant mortality and improving the quality of pregnancy is undeniable. The development of new technologies and equitable access to these services can create a safer future for mothers and babies.



![The role of inositol in the treatment of female infertility [obstetrics and gynecology specialist]](/storage/posts/covers/2026/01/05/c0b071d7095fdcbaa34903c34e092d27a7f5b2fc471de3ff89c0a6eb0c446a10.jpg)

![Children's vaginal infection: symptoms and treatment [obstetrics and gynecology specialist]](/storage/posts/covers/2026/01/05/e56f480f09acfaf71854a94f42ccf293be7e378bd9a4adcffd54d5476bf51caa.jpg)

![Breast cancer [breast] symptoms, diagnosis + treatment [gynecologist]](/storage/posts/covers/2026/01/05/0d2c008b72cfbf5343598c8045fd73cdfbfe6a0e567bd035ea8e1fc90702e96a.jpg)



![Vaginal infection in pregnancy: symptoms, diagnosis and treatment [obstetrician and gynecologist]](/storage/posts/covers/2026/01/05/74fbd328a8a4a83f39778f4a417048ddeb814f527d50d1afc9e23bbe0ad5e371.jpg)