Table of contents
Listen to the summary of this article in the podcast below:
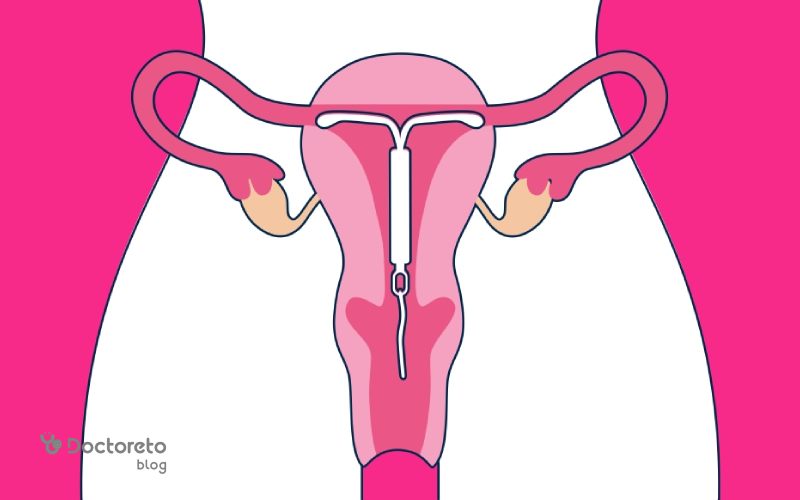
Hormonal IUD (IUD), or contraceptive device, is one of the reliable methods of temporary pregnancy prevention. This device is placed inside the uterus by the doctor. The IUD device can prevent pregnancy for 3 to 8 years. If you intend to get pregnant, you can go to the doctor whenever you want to have it removed. Unlike other methods of contraception, the IUD does not prevent the transmission of sexually transmitted infections (STIs). This prevention method can affect menstruation and make it lighter and simpler.
What is a hormonal IUD device?
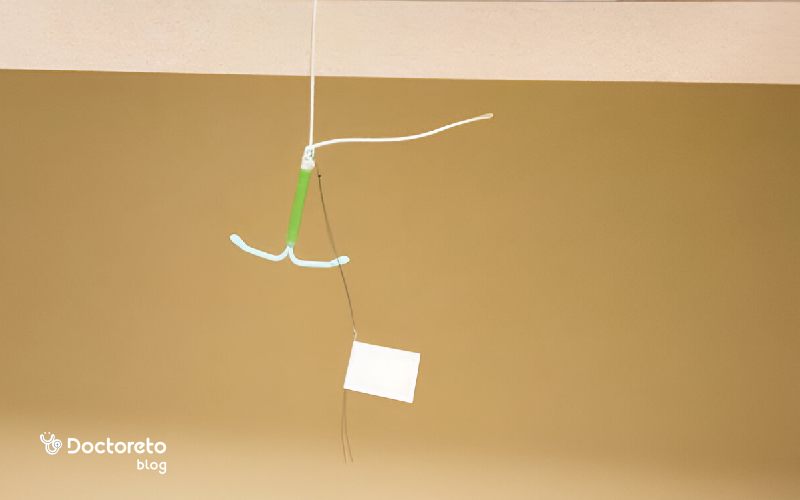
Hormonal IUD is one of contraceptive methods. An IUD is a small T-shaped device that is inserted into the uterus and prevents pregnancy for several years. A hormonal IUD is inserted into the uterus and prevents pregnancy by releasing progesterone. The most famous IUD brand is Mirna, which prevents pregnancy for about 8 years. The rest of the brands can stop in about 3 or 4 years.
Hormonal IUD prevents the fertilization of sperm and egg by releasing a small amount of progesterone hormone. The IUD lasts for several years and prevents pregnancy. If you decide to get pregnant, you can go to the doctor to remove it from the uterus.
How does the hormonal IUD prevent pregnancy?
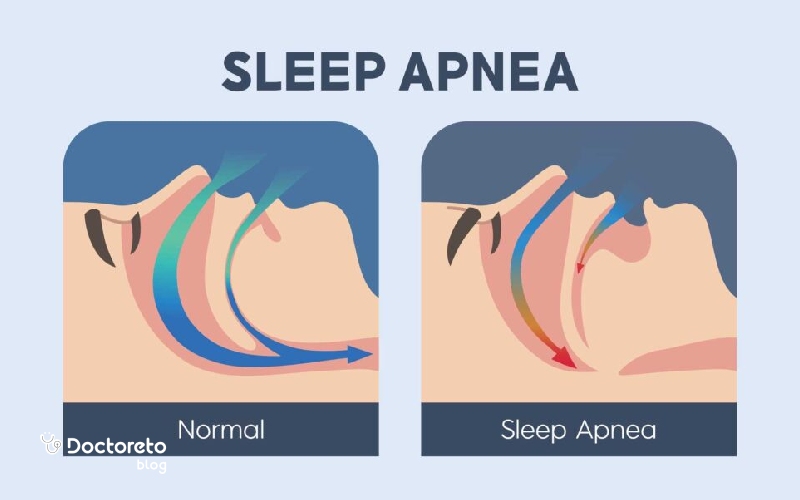
Hormonal IUD keeps the sperm cells away from the egg. When the sperm cannot reach the egg, pregnancy does not occur. The progesterone hormone of this device prevents pregnancy in two ways:
- It thickens the secretions of the cervix (cervical mucus) so that the sperm cannot reach the egg or fertilize it.
- This hormone thins the inner layer of the uterus (endometrium) and partially prevents the release of the egg (ovulation).
How to insert Mirena IUD
Before placing the IUD in the uterus, the gynecologist must perform a pelvic examination. Sometimes it is necessary to take a test to diagnose sexually transmitted diseases. To make sure you are not pregnant, it is better to do a pregnancy test before using the device. One or two hours before the operation, you can use non-steroidal anti-inflammatory drugs such as ibuprofen to reduce pain. The steps to install the IUD device are as follows:
- You lie in the Pap smear examination position; The knees are bent and the legs are open and placed in the holder.
- The doctor may inject local anesthesia near the cervix to reduce pain.
- The gynecologist opens the cervix using a speculum and disinfects this area. The depth of the uterine cavity may also be measured
- You may experience mild to severe cramping when the IUD is inserted.
- The horizontal arms of the IUD should be closed. The device is placed inside the applicator tube and enters the cervix.
- The specialist carefully inserts the IUD into the uterus and removes the applicator tube. The string of the IUD should be shortened enough that it does not protrude from the vagina.

English text:
Inserting an IUD takes fifteen minutes or less. Your provider can perform the procedure during an office visit.
Persian translation:
Intrauterine device insertion takes less than 15 minutes and is done during a regular office visit. noopener">my.clevelandclinic
How to remove hormonal iodine without thread or with thread
To remove the iodine without a thread, the doctor first checks its location with an ultrasound. If the IUD is inside the uterus and not hidden, it can be removed with a special thread tool or the device itself. If necessary, the cervix is opened and a hook or forceps can also be used. If these methods are not successful, referral to a gynecological surgeon is necessary. If the IUD device is not seen in the ultrasound, abdominal imaging is performed.
If it is still not seen, it is possible that the device has been discarded. But if it is determined that the IUD is outside the uterus or in the uterine wall, the patient should be referred to a gynecological surgeon for removal. A tool called forceps is also used to remove the IUD whose thread is known. The doctor takes the IUD thread with this tool and slowly pulls it out. When the IUD arms come out, they bend upwards.

What are the advantages of hormonal IUD?
Hormonal IUD is one of the effective methods and works well in the long term. Among its various advantages, the following can be mentioned:
- About 99% success in preventing pregnancy.
- There is no need to stop sex or use a condom to prevent pregnancy.
- You don't need your spouse's participation.
- It prevents pregnancy for up to 5 years and sometimes even up to 7 years.
- It can be removed from the uterus at any time and get pregnant without any problems.
- It can be used during breastfeeding. Of course, it is better to be placed in the uterus 6 to 8 weeks after delivery.
- It does not have the risk and side effects of birth control methods containing estrogen.
- The amount of bleeding decreases after 3 months.
- Severe menstrual pain and endometriosis pain will decrease.
- Evidence shows that intrauterine hormone may reduce the risk of endometrial malignancy and is accompanied by a minor effect on the reduction of ovarian cyst formation; The evidence for a reduction in ovarian or cervical cancer is not strong.

For whom is the hormonal IUD device not suitable?
Like any contraceptive method, Hormonal IUD is not suitable for some people. You should not use this method of prevention if any of the following apply to you:
- History of breast cancer or suffering from it
- uterine or cervical cancer
- History of sexually transmitted infection (STI) or pelvic infection Liver diseases
- This method is effective in preventing the formation of fibroids; But if you have fibroids, they interfere.
- Pelvic infection or any kind of pelvic inflammatory disease Unexplained vaginal bleeding
- Diabetes or high blood pressure
- Heart disease or history of heart attack Migraine Blood clotting problems or stroke.
What are the types of hormonal IUD?
Different types of hormonal IUD or IUD contraceptive device are available in the market. Different brands all have the same type of hormone and their function in the uterus is the same. But their lifespan is different and they don't last the same:
| Types of IUD | Lifespan |
|---|---|
| Mirna hormonal IUD | 7 years |
| Lilta contraceptive device | 7 Year |
| Kilina IUD | 5 years |
| Skyla contraceptive device | 3 years |
Care after putting Mirna IUD
After the Mirena IUD is inserted, your body needs some time to get used to it. During this time, you may experience symptoms such as abdominal pain, spotting, or mood swings, which are usually normal and will resolve on their own. By following a few simple tips, you can avoid problems and get through this period more easily. Hormonal IUD post-care includes the following:
- For 7 days, avoid having sex, using tampons, washing the vagina or anything that enters the vagina.
- Avoid going to the pool or bathtub for a week.
- Avoid heavy sports for 48 hours to reduce bleeding.
- If you put IUD in the first 7 days of your period, you don't need an additional method of prevention. Otherwise, use a condom for 7 days.
- You may need a visit in the first 6 weeks to check the position of the threads or learn to check the threads yourself.
- In the first months, you may have irregular bleeding or spotting. In some people, menstruation becomes very less or stops over time. Premenstrual symptoms may still be present, even if you are not bleeding.
- If you use a menstrual cup, be sure to release the vacuum before removing it so that it does not move or pull out the IUD.
What is the cause of the decrease of hormonal IUD?
Hormonal IUD displacement is usually caused by normal or severe uterine muscle contractions. The uterus is an active muscle that contracts during the menstrual cycle. In some people, these contractions are so intense that they can push the IUD device towards the cervix and cause it to move or even come out completely. The main causes of iodine displacement are:
- Strong contraction of the uterine muscle, which can pull the IUD down.
- Heavy menstrual bleeding or severe pain, which is accompanied by increased uterine contractions.
- Uneven surface or abnormal shape of the uterus, which may prevent the iud from fitting properly.
- A high level of prostaglandin in the body, a substance that causes the uterus to contract.
- Young age (14 to 19 years old), in this age group, there is a higher probability of iodine protrusion.
Inserting the IUD immediately after delivery, breastfeeding, abnormal position of the uterus, incorrect placement of the IUD, use of a menstrual cup, and the incompatibility of the IUD with the shape or size of the uterus increase the risk of IUD displacement.
How to check a hormonal UD thread?
To check the hormonal IUD thread, you must first wash your hands. Then sit or squat and insert your finger into the vagina until you reach the cervix. The cervix should be firm, similar to the tip of the nose. You should be able to feel the threads.
Do not pull the threads, as this may cause the IUD to dislodge. If you are using a tampon and you don't feel the threads, it is better to check your tampon to be sure of the presence of an IUD. In the first month after placing the IUD, check the threads several times and continue this work after each menstrual period.

What to do if the hormonal thread is not seen?
If the hormonal iodine threads cannot be seen or felt, the iodine may have moved from its place. In this case, you are no longer protected against pregnancy and you may need to use another method of contraception or request emergency contraception in case of possible pregnancy.
If you suspect that the IUD has moved, you should not attempt to reinsert it yourself. The best thing to do is to call your doctor right away to make sure about the condition of the IUD. A doctor can determine for sure if the IUD has moved or not.
Care after hormonal IUD removal
For many women, life goes back to normal after the IUD is removed. It may take a few cycles for periods to settle, and fertility usually returns within a month. If you want to get pregnant, you have to be patient for your body to return to its normal state. Some women may need a little more time to get pregnant, which is completely normal.
After removing iodine, your body may experience some symptoms for some time. From cramping and bleeding to hormonal changes and the return of menstruation, most of these symptoms are temporary and resolve after a few weeks. If you are trying to get pregnant, fertility usually returns quickly, and many women get pregnant after having an IUD removed and have healthy pregnancies.
English text:
quoted from medicalnewstoday
"Mirena is a hormonal IUD that releases the synthetic hormone progestin to prevent pregnancy. Some of the symptoms that people often experience after Mirena placement include: pain, bleeding, and dizziness and missed or irregular periods. although these symptoms should usually go away within about 30 minutes. Some of the symptoms that people often experience after having Mirena inserted are: pain, bleeding and dizziness, missed or irregular periods.”
What are the side effects of the hormonal IUD device?
Hormonal IUD side effects are usually seen for the first few months after insertion. But many people do not experience any of the side effects of hormonal IUDs. The most important side effects of hormonal iodine are:
- Pain and bleeding similar to menstruation (spotting) after inserting it.
- The formation of fluid-filled cysts on the ovaries, which are usually harmless and disappear without treatment.
- Some people have reported headaches, acne, chest pain and mood swings. There is not enough evidence to prove that iodine causes these cases.
- It rarely causes uterine perforation. But using it after childbirth increases the risk of this complication.
If you have never been pregnant before, you have a history of IUD exiting the uterus, or you are under 20 years old, it is better not to use this method. If the side effects of hormonal IUD are severe or if you experience the following symptoms, be sure to contact your gynecologist
- You think you are pregnant.
- You have heavy and continuous vaginal bleeding.
- You have pain during sex.
- You have a fever for no reason.
- You have abnormal or smelly vaginal discharge, lesions and sores.
- You experience a migraine or a severe headache.
- Your skin or eyes turn yellow.
- You have been exposed to a sexually transmitted disease.
- Didn't feel the IUD thread or the thread suddenly got longer.
What is the cause of lower abdominal pain after hormonal IUD?
Lower abdominal pain after hormonal IUD insertion is usually caused by the opening of the cervix, which is done to insert the IUD. This pain is similar to menstrual pain and occurs because the cervix opens to allow the device to pass through. The intensity of this pain can vary from person to person. For some people, the pain may be mild and short-lived, while for others, it can be more severe and prolonged.

What are the side effects of removing a hormonal IUD?
After the Mirena IUD is removed, you may experience cramping and spotting or light bleeding for a few days or weeks. To reduce pain, you can use over-the-counter pain relievers such as acetaminophen or ibuprofen to help you feel better. Other side effects of removing the Ayudi contraceptive device are as follows:
- Bleeding
- weight gain
- Acne
- Breast sensitivity
- fatigue
- Mood swings
- Nausea.
- Prolonged or severe pain in the uterus or abdomen
- Fever
- Heavy bleeding
- Anxiety, depression and mood swings
- Creating a hole in the uterus (although this complication is more related to the placement of the IUD than its removal).
Conclusion and guide to see a doctor
Hormonal IUD is one of the best contraceptive methods. There are different types of IUDs, and in the Mirna type, the device prevents pregnancy by releasing the hormone progesterone. The specialist inserts the device into the uterus with an applicator tube and it can be used for about 5 to 7 years. By using this method, the amount of bleeding and period pain will be reduced. If you don't have children or your age is less than 20 years, it is better to use another method of prevention. After the hormonal IUD is placed in the uterus, you can remove it whenever you decide to get pregnant and get pregnant without any problems. To use this contraceptive method, you must consult a gynecologist.
Your doctor takes care of your health!