The best time for uterine and ovarian ultrasound
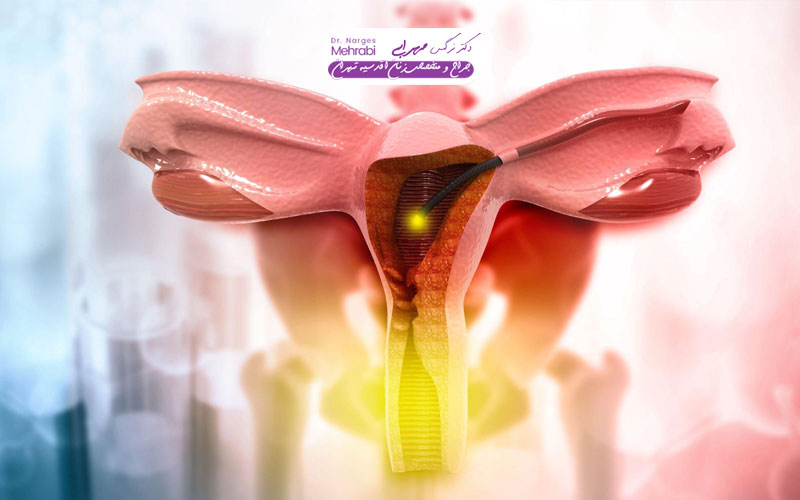
Ultrasound, as one of the non-invasive and highly efficient diagnostic tools in medical science, plays a central role in evaluating the health of women's pelvic organs. This imaging method, using high-frequency sound waves, allows viewing the soft structures of the uterus, ovaries, and fallopian tubes without the need for X-rays or surgical interventions. However, unlike ultrasound of organs such as the liver or kidney, which can be performed at almost any time of the day, the quality and accuracy of information obtained from pelvic ultrasound is strongly affected by physiological changes in the menstrual cycle. inside the uterus) and the ovaries themselves. The thickness of the endometrium varies from the menstrual phase to the luteal phase, and the appearance or disappearance of follicles, corpus luteum, and even temporary cysts are all part of this natural cycle. A thickening of the endometrium, which is considered normal on the eighth day of the cycle, can indicate an abnormality or a polyp on the twenty-fifth day. Therefore, for the specialist doctor and ultrasound technician, the accurate determination of the best time for uterine and ovarian ultrasound is not a recommendation, but a key diagnostic requirement.
The purpose of this article is to go beyond the mere introduction of this imaging technique. We intend to help specialists and clients to avoid repeating unnecessary ultrasounds and achieve the most accurate diagnostic results by choosing the optimal timing by explaining the impact of different stages of the cycle on the ultrasound image. This comprehensive guide will help you understand how the clinical purpose of the referral will be a key determinant in choosing the best time for ultrasound of the uterus and ovaries.
What you are reading
The role of ultrasound in the diagnosis of pelvic diseases and anomalies
The pelvis is the cornerstone of initial evaluations in women and is used for several reasons. This method is a powerful tool for visualizing the anatomy of the pelvis and allows the doctor to examine the size, shape and structure of the uterus (including myometrium and endometrium), cervix and ovaries with high precision. Also, the presence of any free fluid in the pelvis indicates abnormal masses, cysts, or pathological lesions. Therefore, referral to ultrasound is usually done with the aim of accurately diagnosing abnormalities that have caused symptoms such as chronic pelvic pain, abnormal uterine bleeding, or infertility problems.
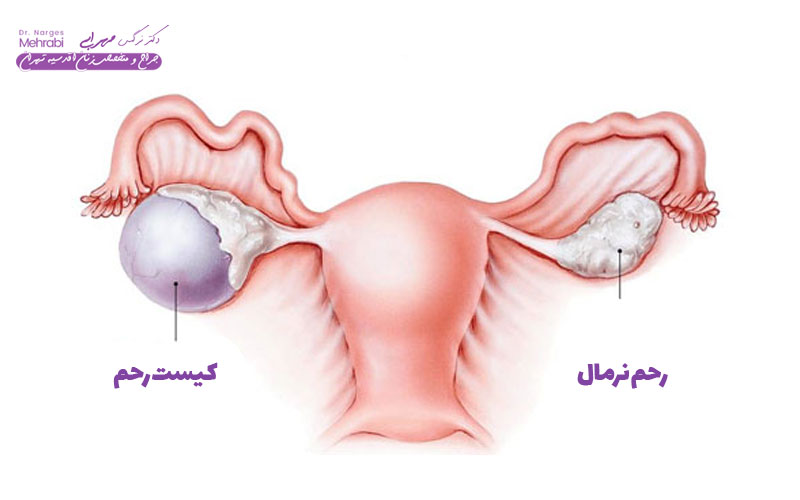
For accurate diagnosis, ultrasound should be performed in conditions where the organs are in their optimal state so that abnormalities can be distinguished from normal changes. For example, the detection of small fibroids (myomas) in the uterus or small ovarian cysts is most effective when the patient's hormonal status interferes with imaging the least. In fact, the ultimate goal of determining the best time for uterine and ovarian ultrasound is to minimize false diagnoses (both positive and negative) that can lead to unnecessary treatments or delays in vital diagnoses.

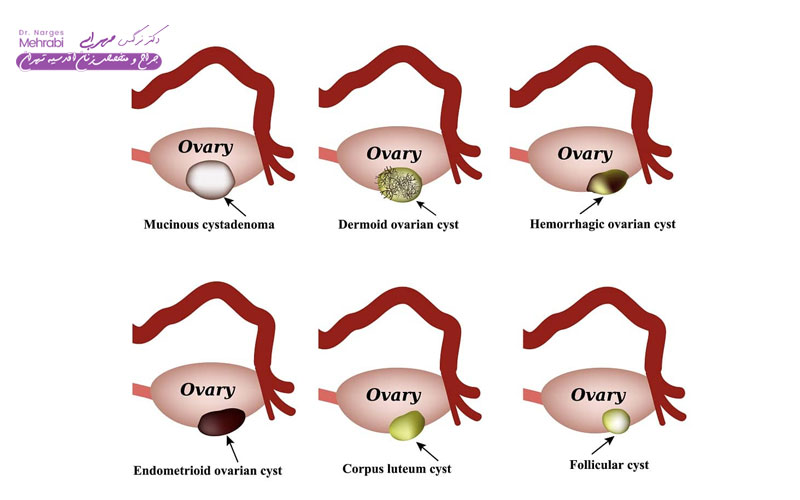
Without proper timing, a normal follicular cyst that develops during the cycle and resolves spontaneously may be mistakenly reported as a pathological mass. Or, conversely, a small polyp in the uterus may be hidden from view due to the thickening of the endometrium in the secretory phase. Therefore, if the purpose of the referral is to investigate a specific abnormality, the specialist should adjust the time according to the patient's physiology so that the imaging is performed in a phase of the cycle when the desired lesion is clearly visible.
In short, ultrasound is not only an imaging tool; Rather, it is a dynamic process whose accuracy depends on the understanding of cyclical changes. Being aware of these changes and consciously choosing the best time for ultrasound of the uterus and ovaries, allows the doctor to determine the patient's pelvic health status with the highest accuracy and make evidence-based treatment decisions. The best time for ultrasound of the uterus and ovaries
The most important factor in determining the best time for ultrasound of the uterus and ovaries is the stage in which the patient is in her menstrual cycle. The menstrual cycle is classically divided into two main phases: the follicular phase (from the first day of menstruation to ovulation) and the luteal phase (from ovulation to the start of the next period). Meanwhile, the menstrual phase, i.e. the first days of bleeding, is often considered the best time window for basic evaluations due to the special condition of the uterus.
During the menstrual phase (usually days 1 to 5 of the cycle), the endometrium, or inner lining of the uterus, sheds and is at its thinnest. This thinness of the endometrium allows the ultrasound technician to examine the inner walls of the uterus with very high resolution and easily detect any small structural abnormalities, such as endometrial polyps or submucosal fibroids (fibroids that protrude into the uterine cavity) that may be hidden when the endometrium is thick.
For this reason, if the purpose of the ultrasound is to evaluate abnormal bleeding or diagnose the cause of infertility, the early days of the cycle (usually days 3-5) are recommended as the best time for uterine and ovarian ultrasound. This timing allows the doctor to get a clear picture of the uterus and make sure there are no lumps in the inner wall that have not grown naturally with hormones. Also, in this phase, the ovaries are also at rest and the number of basal antral follicles can be counted to evaluate the ovarian reserve. Therefore, gynecologists often emphasize that patients visit in the early days of their period. This practice maximizes the accuracy of ultrasound and ensures that pathological structures are distinguished from physiological changes. Failure to comply with this schedule can create the need for ultrasound in the next cycle, which is a waste of time and resources for both the patient and the treatment system.
The best time for ultrasound to evaluate the thickness of the endometrium and polyps
When the main purpose of ultrasound is to accurately evaluate the thickness of the endometrium. (the inner layer of the uterus) and identify abnormalities such as polyps or hyperplasia (excess tissue growth), the importance of timing reaches its peak. In this situation, the purpose of choosing the best time for uterine and ovarian ultrasound is to perform ultrasound in the phase when the endometrium is at its thinnest possible so that the polyps, which are benign masses hanging from the uterine wall, can be seen with maximum clarity inside the uterine cavity. At this time, the endometrium is the least thick due to shedding caused by menstruation and provides a clear space to observe the inner walls of the uterus. Polyps or small fibroids, when the endometrium is thin, appear as clear and uneven bumps on the inner surface of the uterus. If the ultrasound is performed in the luteal phase (after ovulation), the endometrium becomes thick and swollen due to the secretion of progesterone and appears so-called "echogenic" or whiter, and this thickness covers small polyps and makes them almost impossible to detect.

In case of failure to detect polyps or other abnormalities in routine ultrasound in the initial phase, the doctor may turn to Sonohysterography or Saline Infusion Sonography - SIS. This method, which requires thinness of the endometrium, involves injecting a small volume of sterile fluid (saline) into the uterine cavity in the follicular phase. The fluid dilates the uterine cavity and thus contrasts the polyps or other abnormalities with the fluid and significantly increases the diagnostic clarity. Finally, the emphasis on performing ultrasound at this time is to avoid misdiagnosis and the need for repeated ultrasounds. Therefore, if the doctor has requested an ultrasound to evaluate abnormal bleeding or uterine polyp, the best time for ultrasound of the uterus and ovaries is the first few days after the menstrual bleeding has stopped before the endometrium has the opportunity It has not grown again.
The best time of ultrasound to check the health of ovaries and follicles
Checking the health and function of the ovaries is an integral part of pelvic ultrasound, and its timing is different depending on the purpose. If the goal is a general evaluation of the ovaries for possible cysts or masses, the same early phase of the menstrual cycle (days 3-10) as recommended for the uterus is appropriate. At this time, the ovaries are in a state of relative rest, and the functional cysts (cysts that are formed due to the normal cycle) are at their smallest size or completely absorbed, which makes it easier to distinguish them from pathological (abnormal) cysts. Cystic (PCOS) or evaluation of ovarian reserve, the best time for uterine and ovarian ultrasound is still the early follicular phase. In this phase, the number of antral follicles (AFC) in the ovaries is counted. These small follicles are a direct indicator of a woman's ovarian reserve, and counting them early in the cycle, when the dominant follicle has not yet been selected for ovulation, provides the most accurate data. has-link-color" style="border-width:15px">
If the purpose of the ultrasound is to track ovulation to determine the time of intercourse or help with fertility (called folliculometry), the timing must be adjusted precisely based on the growth of the follicles. In this case, ultrasounds begin around day 10 to 12 of the cycle and are repeated every 1 to 3 days until the dominant follicle reaches an approximate size of 18 to 20 mm and the possibility of imminent ovulation is determined. These types of ultrasounds are a serial process, and choosing a single day as the best time for uterine and ovarian ultrasound here is pointless.
In general, early follicular phase is preferable for structural evaluation of ovaries. This timing likely excludes functional cysts (eg, corpus luteum) that may be present in the luteal phase and confound the diagnosis. Understanding these differences and adjusting the time of ultrasound based on the clinical goal (diagnosis or follow-up treatment) is the main key to successful treatment.
Ideal timing for infertility follow-up ultrasounds (folliculometry)
Infertility follow-up ultrasounds or Folliculometry is a precise diagnostic-therapeutic protocol where timing literally determines success. This process aims to monitor the growth of ovarian follicles and the thickness of the endometrium in response to drug treatments or naturally, to accurately predict the time of ovulation. In this way, determining the best time for uterine and ovarian ultrasound in this context, is not a "time", but a "starting point" and "a time sequence".
The starting point for folliculometry is usually in the early follicular phase (days 2 to 5 of menstruation). In this basic ultrasound, the doctor examines the resting state of the ovaries and makes sure that there are no remaining cysts from the previous cycle that can prevent the start of a new cycle. Also, in this ultrasound, the thickness of the endometrium is measured to determine the baseline condition and the number of antral follicles is counted to assess the expected response to drug stimulation.

After starting ovulation stimulation drugs, ultrasounds continue serially. Usually, the first follow-up ultrasound starts around day 8 to 10 of the cycle. From this point on, the best time for uterine and ovarian ultrasound is adjusted every 1 to 3 days. This repetition is critical for daily measurement of dominant follicle growth and endometrial thickening. The goal is to reach the ideal diameter of the follicle for ovulation (around 18 to 20 mm) and the thickness of the endometrium to an acceptable level (usually at least 8 mm).
The best time for ultrasound of the uterus and ovaries The best time for ultrasound of the uterus and ovaries The best time for ultrasound of the uterus and ovaries (such as HCG) or intercourse timing. Here, every 24 hours of delay or haste in the ultrasound can have a direct impact on the failure or success of trying to get pregnant. Therefore, the folliculometry protocol is an excellent example of how the therapeutic goal affects the fine-tuning of the best time for ultrasound of the uterus and ovaries, which requires close cooperation between the patient, the specialist and the ultrasound technician. It
The period of menopause (menopause) creates a special situation in the pelvic ultrasound, because the hormonal cyclic changes have stopped and the pelvic organs are in a static and non-oscillating state. However, even during menopause, determining the best time for uterine and ovarian ultrasound is particularly important, especially if the goal is to evaluate postmenopausal bleeding (PMB), which should be considered a serious warning sign.
In menopausal women, the uterus and ovaries shrink and the endometrium remains naturally thin (atrophic) due to the lack of estrogen. In this situation, the thickness of the endometrium is used as the most important indicator to diagnose the pathology. If a woman experiences bleeding during menopause, the best time for an ultrasound of the uterus and ovaries is immediately during the bleeding period or as soon as possible after. The main goal is to measure the thickness of the endometrium in this condition.
An endometrial thickness of less than 4 to 5 mm in a postmenopausal woman who is bleeding is often considered to be endometrial atrophy (thinning due to hormone deficiency), which is benign. But if the thickness of the endometrium is greater than this limit, especially if the patient is not undergoing hormone replacement therapy, the possibility of endometrial hyperplasia or malignancy (such as endometrial cancer) increases, and the need for follow-up with biopsy or SIS ultrasound is raised. Women on a cyclic HRT regimen (with cyclic estrogen and progesterone) should have their ultrasound done at the end of the progesterone cycle, when the endometrium has shed or thinned in response to the progesterone. For women on continuous combined HRT regimen, the best time for uterine and ovarian ultrasound can be any time, but a baseline thickness should be considered for subsequent follow-ups. Urgent
In situations where the patient presents with acute and urgent symptoms such as severe pelvic pain, unexplained heavy bleeding or bleeding during pregnancy, the principle of the best time for uterine and ovarian ultrasound changes completely. In the emergency, a delay in imaging can lead to serious consequences, so ultrasound should be performed as soon as possible (STAT), regardless of the stage of the menstrual cycle. In these cases, the speed of diagnosis is prioritized over the accuracy due to physiological timing.
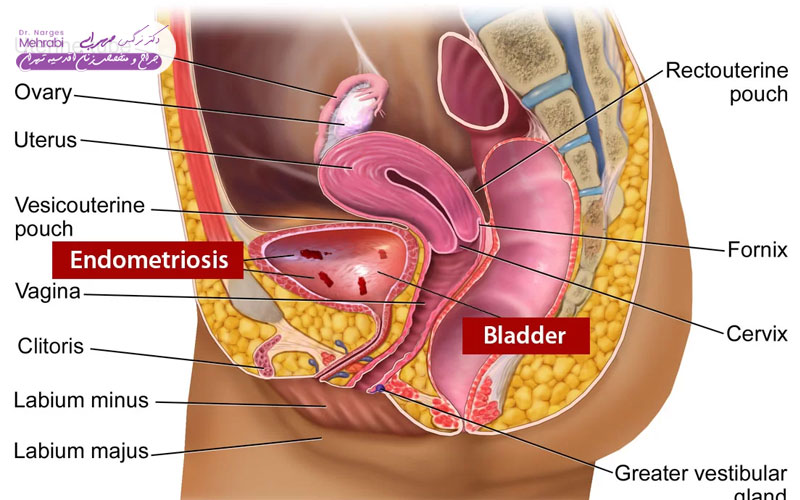
A clear example of this situation is the possibility of ovarian cyst rupture, ovarian torsion or ectopic pregnancy. In cases of ovarian torsion, which is a true surgical emergency and blood flow to the ovary is interrupted, a delay of several hours can result in complete loss of the ovary. Immediate ultrasound can evaluate the state of ovarian blood flow (using Doppler ultrasound) and confirm the diagnosis. In this situation, searching for the best time for uterine and ovarian ultrasound is completely pointless and delay is prohibited.

In case of severe uterine bleeding, an urgent ultrasound is necessary to evaluate the thickness of the endometrium and look for possible causes of bleeding such as large masses, fibroids from childbirth or remnants of pregnancy. Although imaging in the luteal phase or bleeding phase may be less clear, the information it provides about mass size and vascular status is critical to emergency clinical management and helps the physician quickly decide on necessary interventions.
Thus, although cycle timing is important for routine diagnoses, in acute and emergency situations, the urgency of action and rapid diagnosis to prevent serious complications take precedence over all other considerations. has In these cases, the information obtained at any time of the cycle is used as the most vital diagnostic data to save the patient's life or organ health.
Effect of the type of ultrasound (abdominal or vaginal) on determining the best time
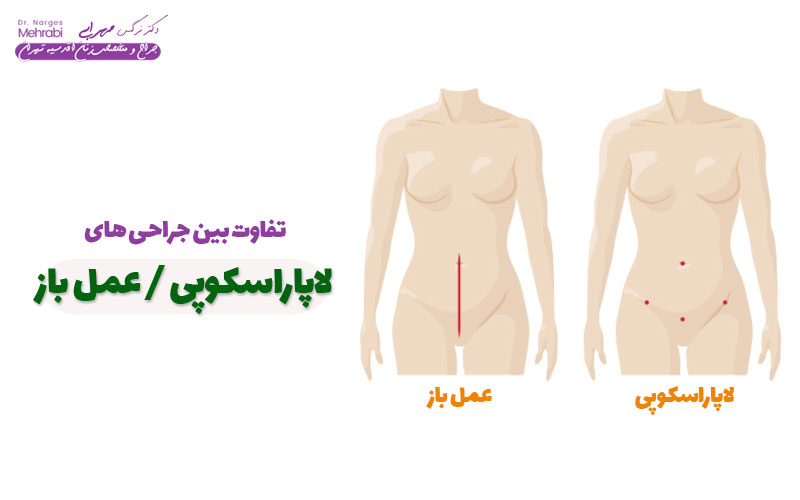
Decision Regarding the type of ultrasound (abdominal or transvaginal ultrasound), it is directly related to determining the best time for ultrasound of the uterus and ovaries and the purpose of the evaluation. Both methods use sound waves, but the entrance path and frequency of the probes are different, which affects the quality of imaging.
The best time for ultrasound of the uterus and ovaries The best time for ultrasound of the uterus and ovaries The best time for ultrasound of the uterus and ovaries The best time for ultrasound of the uterus and ovaries The patient's bladder must be full. The fullness of the bladder acts as an "acoustic window" and removes intestinal gases from the path of the waves and helps to image the large pelvic organs. This method is mostly used to evaluate large uterus and ovaries during pregnancy. Its main limitation is the long distance of the probe from the organs and the use of lower frequencies, which reduces the resolution of details. Because of these limitations, choosing the best time for ultrasound of the uterus and ovaries is less critical in this method, but it is still recommended to follow the menstrual cycle.
In many cases, the doctor uses both methods at the same time. Abdominal ultrasound provides an overview of the entire pelvis and how the organs relate to each other, while vaginal ultrasound focuses on examining microstructural details. Decisions about the type of ultrasound and the best time for ultrasound of the uterus and ovaries should be customized by the specialist based on the clinical situation and imaging goals.
Conclusion
Uterine and ovarian ultrasound is a dynamic and time-dependent diagnostic process whose success is more than any other. It depends on understanding the physiological changes in the menstrual cycle. Determining the best time for uterine and ovarian ultrasound is not a simple act; Rather, it is a clinical decision that considers the purpose of the assessment. In general, to evaluate the internal structures of the uterus such as polyps and endometrium, the early follicular phase (day 3 to 10 of the cycle), when the endometrium is at its thinnest, is preferable. This timing minimizes the possibility of error and repetition of ultrasound and maximizes the resolution of imaging (especially with the transvaginal method).
In special conditions such as infertility follow-up (folliculometry), the timing becomes a serial protocol that starts from the beginning of the cycle and continuously repeats the growth of the egg until the moment of ovulation. On the other hand, in emergency situations such as acute pain or severe bleeding, the principle of physiological timing is completely abandoned and ultrasound should be done immediately so as not to endanger the patient's health. This diversity in timing shows the flexibility and high importance of this diagnostic tool in different clinical situations.
The best time for ultrasound of the uterus and ovaries The best time for ultrasound of the uterus and ovaries The best time for ultrasound of the uterus and ovaries refer to Understanding how hormonal changes affect the image provided by ultrasound helps the patient to be more informed in his treatment path and ensure accurate and timely diagnoses. href="https://drmehraabi.com/%d8%af%da%a9%d8%aa%d8%b1-%d9%85%d8%aa%d8%ae%d8%b5%d8%b5-%d8%a7%d9%86% d8%af%d9%88%d9%85%d8%aa%d8%b1%db%8c%d9%88%d8%b2-%d8%af%d8%b1-%d8%aa%d9%87%d8%b1%d8%a7%d9%86/">
FAQ
If I have irregular periods, what is the best time for an ultrasound of the uterus and ovaries?
If you have irregular periods, which may be a sign of hormonal disorders such as polycystic ovary syndrome (PCOS), it is recommended to have an ultrasound at Let's say you haven't bled for a few weeks. Otherwise, the best time for a baseline assessment is in the early days of bleeding (days 3-5), although the onset may be unexpected. In cases of prolonged non-bleeding, the doctor may recommend an ultrasound at any time to check the condition of the endometrium. The main goal is to have the endometrium in a relatively stable position for evaluation.
Does the bladder need to be full for transvaginal ultrasound?
No, for transvaginal ultrasound (TVS), The bladder must be completely empty. The fullness of the bladder, which is necessary for abdominal ultrasound, in vaginal ultrasound, moves the pelvic organs away and causes discomfort and reduces the quality of imaging. Only if a simultaneous abdominal ultrasound is required, you may be asked to drink some fluids, but for the vaginal part, the bladder must be emptied. 10th?
Yes, an ultrasound can be done in the luteal phase, but this is not the best time for ultrasound of the uterus and ovaries to detect polyps or small endometrial lesions. In the luteal phase, the endometrium thickens and a temporary cyst called corpus luteum appears in the ovaries, which may be confused with pathological cysts. Ultrasound in this phase is usually performed only in emergency situations or to check the corpus luteum and confirm ovulation.
When is ultrasound of the uterus and ovaries recommended for pregnant women?
Uterine ultrasound and Ovary during pregnancy is routinely recommended in several stages. The first ultrasound is performed between 6 and 9 weeks of pregnancy to confirm the intrauterine pregnancy and determine the heart rate. NT ultrasound (evaluation of folds behind the neck of the fetus) in weeks 11 to 14 and ultrasound anomaly scan (checking for abnormalities) in weeks 18 to 22 are performed as the best time for ultrasound of the uterus and ovaries during pregnancy (focusing on the fetus). Subsequent ultrasounds are determined depending on the doctor's needs.
What happens if I go for an endometrial ultrasound at an inappropriate time?
If for endometrial evaluation (such as polyp detection) at an inappropriate time of the cycle (luteal phase or when the endometrium is thick), small polyps may be hidden by the thickness of the endometrium and go undetected. This can lead to misreporting of ultrasound and failure to diagnose the cause of abnormal bleeding. As a result, the doctor will probably request a repeat ultrasound at the best time for uterine and ovarian ultrasound (early follicular phase).
Is transvaginal ultrasound safe during menstrual bleeding?
Yes, transvaginal ultrasound during menstrual bleeding is completely safe and has no medical contraindications. In fact, as mentioned in the article, days 3-5 of the cycle (when there is usually still light bleeding) are often considered the best time for an ultrasound of the uterus and ovaries to evaluate the thickness of the endometrium and small polyps, because the endometrium is at its thinnest.
Best time for an ultrasound of the uterus and ovaries Ultrasound of the uterus and ovaries
The best time for an ultrasound of the uterus and ovaries.
This article is being updated and expanded to meet SEO standards.