PRP and microneedling in cosmetic medicine
PRP and microneedling in cosmetic medicine
principles and methods of performing PRP (platelet-rich plasma)
1
PRP: mechanism and practical considerations
Abstract
Platelet rich plasma (PRP) has many potential applications in skin diseases. PRP is autologous, meaning it is taken from the patient's own blood and spun in a centrifuge to produce a final plasma product with a high concentration of platelets. These platelets then activate and release key growth factors that ultimately begin to send cascading signals to maximize tissue repair and rejuvenation.
Many systems are available for obtaining PRP. It is very important that these systems (devices) are evaluated objectively and all factors required for the patient as well as the setting in which PRP will be used are considered.
Key words: platelet-rich plasma (PRP), plasma therapy, mechanism of action, evaluation of separation systems, preparation, practical considerations
| Key Points |
| Platelet-rich plasma has several uses for the skin. The full understanding of its mechanisms of action remains unknown. However, the stimulation of the growth factors inside the platelets has an essential role. Several platelet transfer and separation systems are available in the market. It is very important to evaluate and understand the advantages and disadvantages of these separation systems. |
1.1 Introduction
Interest in the use of autologous platelet-rich plasma (PRP) has increased for the management of a variety of clinical cases. PRP PRP was first applied for use in tissue repair and homeostasis in many medical and aesthetic conditions, including orthopedics, dentistry, plastic surgery, and dermatology as seen in Table 1.1. In several studies and researches, the effectiveness of PRP in androgenetic alopecia, skin rejuvenation and hair transplant surgery has been evaluated.
| Table 1.1 Use of PRP in skin and other medical cases |
| Applications of PRP in the skin | Applications of PRP in other fields of medicine |
| • Androgenetic alopecia • Surgery to improve scars or pimples • Acne and scars • Skin rejuvenation • Skin strengthening • Stretch marks or stretch marks • Skin aging • Wrinkles • Melasma or facial spots • Hair transplant surgery • Dark circles usually in the area around the eyes | • Tendon injuries • Muscle injuries and wounds • Bone changes and renewal • Arthritis • Bone grafting • Sinus lift surgery • Fat injection • Mammoplasty or breast reconstruction surgery • Scar reconstruction • Jaw and bone reconstruction surgery • Repair of oral wounds • Dry eye syndrome • Ocular surface syndrome after LASIK surgery |
| Abbreviation: PRP, platelet-rich plasma. |
However, there are very few randomized controlled trials in this field that are of poor quality. It can be said that with the increasing penetration of PRP in cosmetic procedures, it is important to understand what PRP is and its mechanism of action. The process of PRP preparation must be fully understood in order to effectively differentiate between the types of separation systems available.
2.1 Definition of Platelet Rich Plasma (PRP)
Plasma therapy or PRP is an autologous preparation of plasma with a high concentration of platelets, which is taken from a person's blood. The range of normal blood levels is 150,000 to 400,000 µl, or 150 to 400 x 109 L/L.
Today, the working definition of PRP is plasma containing more than 1,000,000 platelets/microliter, based on studies that show increased bone and soft tissue healing at this level. Most PRP preparations have a concentration 4 to 8 times higher than peripheral blood, depending on the preparation system. Studies have shown that growth factors in PRP increase linearly with increasing platelet concentration. Giusti and his colleagues mentioned the induction of vascularization in endothelial cells, which was optimized with a platelet concentration of 1,500,000 platelets/microliter. In addition, based on this research, it was determined that very high concentrations of platelets have actually reduced vascularization. This negative correlation is also observed in studies that show the effect of an inhibitor on bone regeneration with very high platelet concentrations. The use of autologous PRP preparations has several advantages. Among other things, it lowers the possibility of immune reactions and disease transmission is unlikely.Therefore, this method is completely safe, well tolerated and has minimal side effects.
PRP PRP is physiologically different from recombinant growth factors and as a result it contains "pure" growth factors.
In addition, they are transported through a clot, which is considered the natural transport system in humans. Recombinant growth factors are extracted from an external system, usually from other animals, and transferred through artificial carriers. Plasma therapy includes leukocytes (white blood cells), which are both catabolistic and pro-inflammatory, along with platelets and plasma, which cause anabolism functions in the body. It is important to note that these are seemingly opposing functions that are properly balanced, allowing each to fulfill its purpose. Even small changes in the levels of these growth factors can create an imbalance, causing increased inflammation or pain. It is hypothesized that maintaining a net balance of anabolism and catabolism functions helps to maintain a favorable environment for tissue healing and growth.
The scientific basis of PRP and the proposed mechanism of action of PRP
The mechanisms of PRP are not fully understood. However, platelets are believed to release protein signals, including a large number of growth factors, chemokines, and cytokines, that induce cell proliferation and differentiation. Platelets contain more than 20 growth factors within their alpha granules, which are released after activation to transport signaling molecules into the surrounding tissue.Table 2.1 lists important growth factors such as platelet-derived growth factor (PDGF), transforming growth factor (TGF), epidermal growth factor (EGF), vascular endothelial growth factor (VEGF), insulin-like growth factor (IDGF), and interleukin 1 (IL-1) (Table 2.1).
| Table 2.1 PRP growth factors and their primary functions |
| growth factors | function |
| PDGFαα, PDGF αβ, PDGF ββ | • chemotaxis for fibroblasts, macrophages (xenophages) and neutrophils • mitogenic for fibroblasts, smooth muscle cells, Endothelial, mesenchymal cells, and osteoblast • Encouraging the synthesis of collagen and other proteins, regulating collagenase enzyme secretion |
| TGF-β1, TGF-β2, TGF-α | • Encouraging vascular formation • Regulating cell proliferation, differentiation and apoptosis • Chemotactic of fibroblasts, keratinocytes and macrophages • Fibroblast mitogen, smooth muscle cells • Inhibition of endothelial cells, keratinocytes, lymphocytes and macrophage proliferation • Regulation of matrix proteins (collagen, proteoglycan, fibronectin, and matrix degrading proteins) • Proliferation of undifferentiated mesenchymal cells |
| VEGF | • Stimulation of vascularization and vessel permeability • Chemotactic and mitogen of endothelial cells |
| FGF-2, FGF-9 | • Help in tissue regeneration • Stimulate the growth and differentiation of mesenchymal cells, chondrocytes, osteoblasts |
| EGF | • Strongly in regulating proliferation, differentiation and Cell survival is involved • stimulation of vascular formation • mitogen of fibroblasts, endothelial cells, mesenchymal cells and keratinocytes • stimulation of endothelial chemotactic • regulation of collagenase secretion |
| IGF-1 | • regulation of cell metabolism • stimulation of proliferation and differentiation in osteoblasts (bone formation) • Chemotactic of fibroblasts • Stimulation of protein synthesis |
| CTGF | • Stimulation of vascularization, cartilage regeneration, fibrosis and platelet adhesion |
| Abbreviations: CTGF, connective tissue growth factor; EGF, epidermal growth factor; FGF, fibroblast growth factor; IGF, insulin-like growth factor; PDGF, platelet-derived growth factor; PRP, platelet-rich plasma; TGF, transforming growth factor; VEGF, vascular endothelial growth factor |
This process mimics the mechanisms required for skin applications, causing changes at the microscopic level including vascularization, collagen synthesis, extracellular matrix production and apoptosis reduction.
The proposed mechanism of PRP in medical dermatology varies depending on the situation of its use. As noted, the growth factors released by platelets in PRP may stimulate different targets based on the specific treated areas.
1.3.1 Mechanism of action of PRP effects on hair growth
Plasma therapy stimulates hair growth through many mechanisms, but one important pathway is vascularization associated with anagen, or the active phase of hair growth.
Countless treatments for hair loss have been performed with the aim of increasing blood vessels and improving blood flow in the hair follicle unit. Vascular endothelial growth factor (VEGF) secretion is largely responsible for anagen-associated vascularization and has also been shown to promote growth of dermal structures.
Beyond VEGF, alpha granules in PRP release increased levels of PDGF and platelet-derived endothelial growth factor. According to the hypotheses, these factors work on the stem cells of hair follicles and stimulate new angiogenesis. Likewise, PRP has been used to effectively treat male and female hair loss (Figure 1.1). Improved circulation in these structures occurs immediately after the surrounding hair follicles show a clear mechanism of improved hair growth. Similarly, subcutaneous injections of PRP improve the survival of skin grafts, possibly by a mechanism similar to increased blood flow.
There are many other mechanisms by which PRP may promote hair growth. Li and colleagues showed that increased levels of beta-catenin, extracellular signal-related protein kinase, and AKT signaling all contribute to dermal papilla cell proliferation. Activated plasma increases the levels of phosphorylated extracellular signal and regulates protein kinase and phosphorylated Akt, molecules that lead to dermal papilla proliferation and proliferation in humans. Interestingly, the PRP effects found in this study show the importance of achieving the appropriate levels of plasma therapy to achieve maximum results.
Countless studies have detailed PRP and its anti-apoptotic effects. This mechanism is based on the ability of PRP to induce Bcl-2 activation as well as AKT phosphorylation (which are involved in anti-apoptotic regulation).
Dermal papilla cells are protected from disruption and premature loss and remain active, thereby extending the anagen phase of the hair cycle and delaying catagen induction into the telogen or resting phase.
In addition, Lee and colleagues found that PRP treatment nearly doubled the transcriptional activity of beta-catenin, which is expressed in the hair follicle during the anagen phase. This process, along with the ability of plasma therapy or PRP to regulate and improve fibroblast growth factor 7 (FGF-7), also helps to lengthen the anagen or growth phase of the hair cycle. Finally, induction of FGF-7 signaling has also been shown to stimulate the differentiation of stem cells from hair follicles.Mechanism of action of PRP in rejuvenation and repair
As with hair growth, there are likely several mechanisms through which PRP affects skin rejuvenation. Accumulated fragmented collagen fibrils or strands prevent the growth of new collagen and lead to disruption of the extracellular matrix. Activated plasma increases the expression of matrix metalloproteinases (MMP-1 and MMP-3) by stimulating the regeneration of the extracellular membrane and removing damaged collagen fragments, ultimately allowing the recovery of more regularly organized collagen synthesis. Plasma therapy (PRP) contains several growth factors that stimulate human skin fibroblasts and strengthen collagen production and regeneration. In addition, it has been shown that it increases the secretion of hyaluronic acid. Among its many functions in the field of skin, hyaluronic acid is strongly related and dependent on water, and therefore increases skin volume and hydration. Collectively, these findings suggest that PRP solution may enhance and increase extracellular matrix synthesis and is a possible treatment for skin rejuvenation and scarring and acne.
Plasma therapy (PRP) has recently been used to treat acne and facial scars by reusing ablative lasers. It has also been used in the field of wound care after abrasion laser treatment. Reapplication of the fractional carbon dioxide laser (fractional CO2) has been shown to cause similar damage to normal wounds.

Image 1.1 Platelet rich plasma (PRP) used in female hair loss, before and after. Patient 1 (a) before PRP and (b) 4 months after treatment. Patient 2 (c, d) before PRP and (e, f) 4 months after treatment.
Thus, the addition of platelets, as a key element for normal wound healing, should help and accelerate tissue regeneration after laser ablation treatment. While currently unproven, it is believed that the release of PRP from alpha granules (containing large storage pools of growth factors) leads to more efficient and faster tissue healing. In addition, the use of PRP has resulted in faster wound healing, reduced erythema, and decreased water loss in patients' skin after receiving fractional ablation laser.
Preparation options
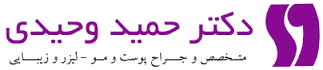
The concept of PRP relies on the centrifugation of whole blood and the separation of desired components based on their specific gravity. PRP preparation can be done manually or with an automatic machine. However, the main process begins with drawing peripheral blood from the patient (Figure 2.1 a-e). Then the tubes of blood (often containing blood anticoagulant) are spun in a centrifuge according to specific protocols by adjusting the speed, rotation period, and spin time.
The rapidly rotating layers of different blood cell lines are based on the accumulated mass in the same way that platelets are in plasma, and for this reason it is called platelet-rich plasma (PRP) and it is extracted from tubes with variable concentrations of red blood cells and granulocytes (Figure 3.1). In some protocols, activators are added before use (read the text below).
The two main methods of manual plasma preparation are the "PRP production" method and the "buffy coat" method. In the "PRP production" method, the whole blood is subjected to an initial slower centrifugation, called "soft spin", which produces an upper layer consisting of platelets and leukocytes, a middle layer, called the buffy coat (which is rich in white blood cells {WBC}), and a lower layer, containing mostly red blood cells (RBC). The upper layer and the surface buffy coat layer are then extracted and subjected to a second round of centrifugation at a higher speed, called "hard spin". This process results in the formation of soft pellets consisting mainly of platelets along with platelet-poor plasma (PPP), which are then removed, leaving the PRP plasma.
In the "buffy coat" method, whole blood is first separated in a heavy spin process as an upper layer of PPP, a middle layer (containing PRP), and red blood cells or RBC underneath. The plasma on the surface is removed, then the buffy coat is given a gentle rotation, pure plasma and leukocytes are produced, and the leukocytes are discarded.
Currently, there are several commercial automated PRP production systems, which facilitate the production of platelet-rich plasma (PRP) in an efficient and simple process. Automated systems use sensors to detect the interface between buffy coat and red blood cells (RBC). This process is caused by the continuous concentration of PRP.Each system has a different method to collect and concentrate platelets. Generally, 30 mL of whole blood yields 3 to 5 mL of PRP (depending on the patient's platelet level, system, and technique used). The results of automatic PRP production are not permanent, but they are more repeatable or reproducible than manual methods. Additionally, closed systems reduce potential errors and help ensure sterile conditions are maintained throughout treatment.
Before injection, PRP is often activated by adding thrombin or calcium chloride. After activation, PRP must be used immediately to maintain its viability. Some systems do not require this step because collagen is the natural activator of PRP and therefore exogenous (external) activation is not required when used in soft tissue.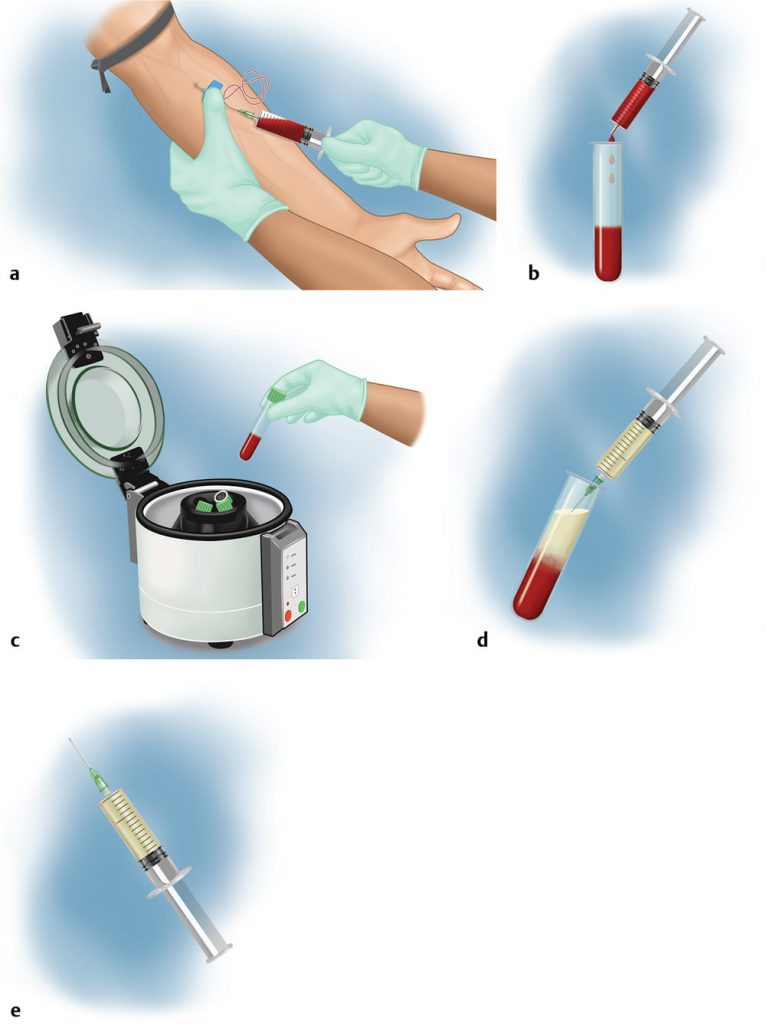
Image 2.1 Procedures for collecting platelet-rich plasma (PRP) using a single-centrifuge method. (a) Step 1: Blood collection – venipuncture from the brachial vein. (b) Step 2: Transfer blood to collection tubes for centrifugation. (c) Step 3: Placing the samples inside the centrifuge. (d) Step 4: removing the PRP layer with a syringe after the centrifugation step. (e) Step 5: PRP injection with a syringe after preparation.
Image 3.1 Composition of whole blood and platelet-rich plasma
1.5.1 Important considerations when evaluating PRP systems
There are many variables to consider when choosing to evaluate a PRP preparation system. Currently, each available proprietary system varies according to their preparation method. There is no guideline or standard regarding the proper technique to achieve the desired platelet concentration in PRP preparations, and this issue makes comparison and evaluation of systems difficult. However, certain criteria should be considered when determining which one to use in said practice setting.
It is important to consider the concentration of platelets produced by each system. While the optimal concentration for skin or plastic surgery recommendations is still unknown, different systems produce highly variable solutions.
As mentioned earlier, a minimum of 1,000,000 platelets per microliter has been shown to be required for wound healing and 1,500,000 platelets is desirable for angiogenesis (Table 3.1).
The effect of white blood cells (WBC) in PRP is highly debated. Many believe that white blood cells, or WBCs, are important components of PRP because of their antimicrobial properties that protect against infection and allergies. Others believe that platelets already have antimicrobial properties and therefore WBCs are unnecessary. In fact, it has been suggested that the presence of high levels of WBCs, especially neutrophils, may also be detrimental to the healing process. Neutrophils cause inflammation, potentially damaging healthy tissue, resulting in unwanted fibrosis, scarring, and a catabolism cascade.
In addition, concentrated leukocytes can neutralize many growth factors released in their vicinity. Studies have shown that these effects hinder wound healing. In the same way, Sandman and his colleagues, in addition to the concentration of platelets, also considered the degree of effect of plasma therapy or PRP on the appropriate amount of platelet collection in WBC.
| Table 3.1 Comparison of preparation systems |
| System | Average platelet concentration Formula(×10^9/L) | Average white blood cells or WBC Formula(×10^9/L) | Average neutrophils Formula(×10^9/L) | Average red blood cells Formula(×10^9/L) Control 269 8.73 5.5 4.7 Magellan (Arteriocyte Medical) 1266 31.4 15.1 1.03 GPS III (Biomet) 964 35.8 15.4 1.03 ACP (Athrex) 412 1.3 0.4 | 0.0333 |
| SmartPrep2 (Harvest) | 1224 | 24.7 | 6.47 | 1.43 |
| Source: Adapted from Fitzpatrick, J, Bulsara, MK, McCrory, PR, Richardson, MD, Zheng, MH Analysis of variations in extraction of platelet-rich plasma and blood components between 4 common commercial kits. Orthop J Sports Med. 2017 |
In the plasma therapy method, a shorter and slower cycle is used with the aim of removing white blood cells, instead of losing some platelets. In the buffy coat method, a longer rotation with a higher degree is used to create a concentration layer and capture as many platelets as possible. Red blood contains reactive oxygen species, which cause unwanted inflammatory reactions at the injection site. RBC, or direct injection of red blood cells into the tissue, may lead to increased swelling and pain for the patient. In addition, inflammation has a negative effect on hair regrowth and creates a catabolism environment that does not stimulate regeneration and hinders the effect of growth factors; It may also induce telogen effluvium as an unintended consequence. Several studies have shown that despite similar preparation techniques, each system produces variable amounts of WBCs and RBCs (▶ Table 3.1)
Similarly, more studies are necessary to compare different systems.
When comparing systems, it is very important to note that different devices that use different volumes do not measure the concentration reliably. As such, the preparation of systems should always be evaluated using the dose or total amount of platelets. In addition, because platelet dysfunction reduces growth factor production, it is critical to find a system that produces healthy platelets. The time and duration of rotation, the acceleration and speed of centrifugation, and the distance between proteins are all important and determining factors in creating the quality and, as a result, the effectiveness of PRP. Other factors worth considering include the centrifuge rotor (ease and smoothness of rotation), anticoagulants used or tools used to prevent platelet aggregation (for example, acidification can affect both ease of injection and platelet quality), and minimization of platelet gradients. Effective and efficient conditions for platelet recovery are low centrifugation acceleration (about 100×g, 10 minutes) in the first rotation and about 400×g in the second rotation to avoid the effects of platelet activation.
There is much conflicting information regarding the efficacy of single-spinning versus double-spinning PRP preparations in the centrifuge. In theory, single spin (plasma methods) should produce lower concentrations of platelets than double spin (buffy coat) methods. While there are studies that have shown that systems with one spin centrifuge are more effective in concentrating platelets in the PRP method to sufficient levels.
It should also be noted that both studies have high standard deviations, indicating high levels of variation. There are several systems available that use different rotation methods. For example, Eclipse and RegenLabs use the single spin (centrifuge) method (Figure 2.1a-e).
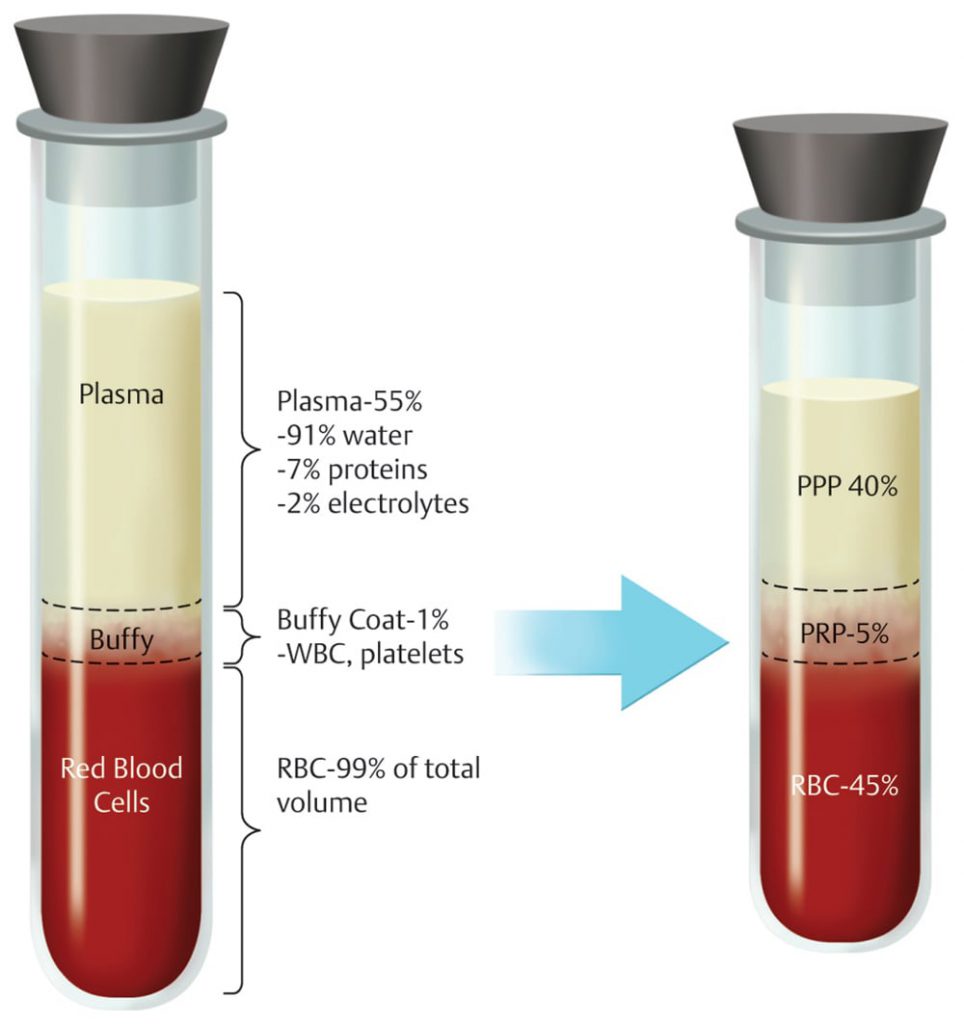
In addition, manufacturers of new systems currently on the market claim that these systems are capable of performing double spin in a single centrifuge (▶ Fig. 4.1a-e).
Figure 4.1 Collection of platelet-rich plasma (PRP) using an automated system. (a) Step 1: Syringe, butterfly needle (Venn scalpel), tourniquet, and anticoagulant for blood collection. (b) Step 2: Blood sampling from the veins of the arm. (c) Step 3: blood mixed with anticoagulant ready for centrifugation. (d) Step 4: Centrifuge the blood. (e) Step 5: PRP is ready for injection.
Using PRP in a beauty field has unique requirements compared to other specialties.
The amount of PRP produced depends on the volume of blood taken and the capacity of the centrifuge in each rotation.
Orthopedic and other surgical systems require the circulation of large amounts of blood to produce the volume required for extensive surgery. This method may be suitable for use during reconstructive or plastic surgery in the operating room. However, skin care and in-office applications generally require approximately 5 to 12 mL of PRP, so finding a system that circulates a smaller volume of blood is essential. However, small vials have limited concentration capacity since only a fraction of the drawn blood is converted to PRP, and in general, the more concentrated the solution, the lower the overall performance. The size of the centrifuge, the cost of the consumables, and the time required for collection and processing must also be considered. In ambulatory operations, compact centrifuge systems are preferred over hospital operating room systems that have less space limitations. Consumables costs must be considered given multiple treatment protocols for many skin conditions. Likewise, maintaining a reasonable cost is important to ensure the feasibility and long-term viability of patients' treatment protocols. A shorter turnaround time is also desirable.
Manual systems are of interest to doctors because their price is cheap and their goal is to achieve high PRP concentration. However, these systems are highly technique-dependent and prone to contamination, prone to damage to platelets, and require more manpower for thorough and timely preparation. Although more expensive, automatic systems simplify the preparation process, minimize damage to platelets, and reduce the possibility of contamination.
6.1 Conclusion
The use of PRP in skin beauty and plastic surgery has increased. PRP is an autologous solution that contains concentrated platelets that activate and stimulate growth factor cascades and induce vascular regeneration, tissue regeneration, and anti-apoptotic pathways. It is important to understand the advantages and disadvantages of different preparation systems and to identify which methods produce the highest yield and best quality PRP. Future randomized clinical studies will describe the role of PRP in many cosmetic applications. It is likely that the ideal system will vary based on clinical circumstances.




