Physiotherapy of pelvic varices
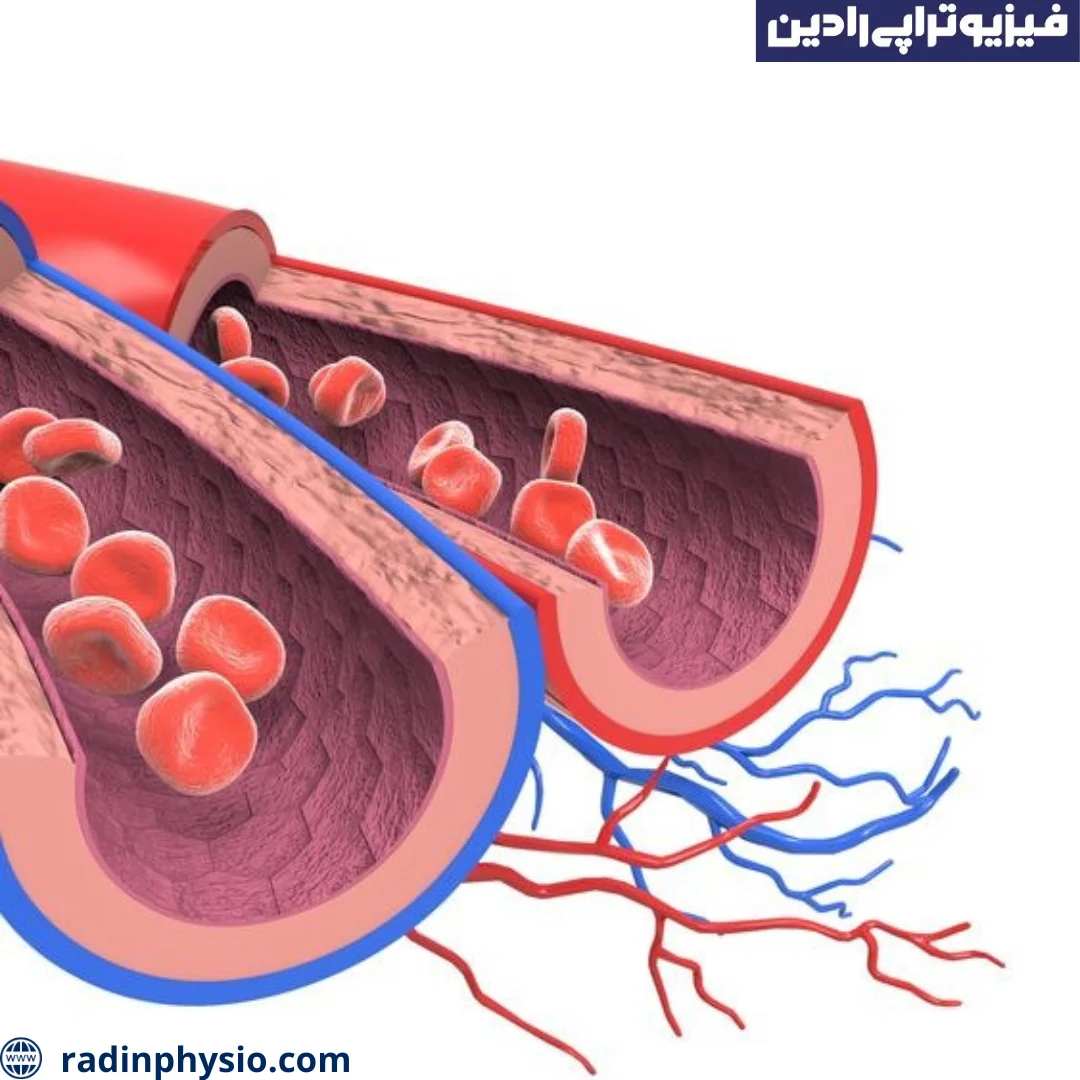
Pelvic Varicose Veins is a medical condition in which the pelvic veins are affected. Pelvic veins carry blood from the lower body to the heart. When these veins are distressed or swollen, pelvic varices occur.
The causes of pelvic varices may include excessive pressure in the pelvic veins, damage to the venous valve system, decreased blood flow, and dysfunction of the lymphatic system. Some possible factors that cause pelvic varices include pregnancy, old age, obesity, insufficient physical activity, hormonal imbalance, hereditary factors, and pelvic traumas.
Symptoms of pelvic varices may include pain, swelling, heaviness, and tenderness in the pelvic area. In case of symptoms of pelvic varices or worsening of existing symptoms, it is recommended to see a doctor. The doctor may make a more accurate diagnosis based on imaging using imaging methods such as ultrasound, computed tomography (CT scan) or angiography.
Treatment of pelvic varices may include lifestyle changes, medications, physical therapy, and in some cases, surgical procedures such as ligation and osteotomy. Your doctor will determine the best treatment method for you based on the severity of your symptoms, imaging-based factors, and other relevant factors.

What are the causes of pelvic varicose syndrome?
Pelvic Varicose Vein Syndrome is a rare medical condition and its exact causes are still not fully understood. But some of the possible factors that cause pelvic varicose syndrome are:
- Genetic factors: Having a family history of pelvic varicose syndrome can be an important factor in the occurrence of this condition. The heredity of several factors that cause defects in venous blood flow can be traced.
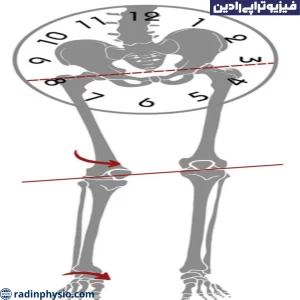
- Structural and functional defects: Some people may be born with structural or functional defects in the pelvic venous system. These defects may reduce blood flow and increase pressure in the pelvic veins, resulting in pelvic varicose syndrome.
- Environmental factors: Some environmental factors can play a role in the occurrence of pelvic varicose syndrome. Such as pelvic traumas, infections, seizures, high pressure in the pelvic area and drug use.
It is important to know that for most cases of pelvic varicose syndrome, the exact cause is not known and there is a need for more research in this field. In case of symptoms of pelvic variceal syndrome or related questions, it is recommended to see your doctor so that an accurate diagnosis and appropriate treatment can be provided.
The cause of pelvic varices in pregnancy
Pelvic varicose veins are very common in pregnancy and its cause is related to the following factors:
Increasing blood volume
During pregnancy, the volume of blood in a woman's body increases to meet the needs of pregnancy. This increase in blood volume may increase the pressure and tension in the pelvic veins and cause pelvic varicose veins.
Progesterone hormone increase
During pregnancy, the level of progesterone hormone increases in the woman's body. This hormone causes the veins to dilate and open, including the pelvic veins. These changes in pelvic veins may lead to pelvic varicose veins.
pressure on pelvic veins
During pregnancy, the pressure on the pelvic veins increases due to the growth of the uterus and more pressure on the vessels in the pelvic area. This pressure may disrupt blood flow and cause varicose veins in the pelvis.
Structural changes of veins
In pregnancy, some structural changes occur in the veins. The growth of the uterus and the increase in pregnancy weight cause more pressure on the pelvic veins and can lead to pelvic varices. A combination of these factors may cause pelvic varices in pregnancy. If you are experiencing symptoms of pelvic varices during pregnancy, it is important to consult your doctor. He or she can provide guidance on symptom relief, lifestyle changes, and appropriate treatment if necessary.
What are the symptoms of pelvic varices?
Symptoms of pelvic varices may be diverse and depend on the severity and location of the disorder. Some of the symptoms of pelvic varices are:
- Pain: Pain in the pelvic region and pelvic chest area can be one of the common symptoms of pelvic varices. This pain usually varies in intensity and duration and may be felt as sharp, burning or a combination.
- Swelling: Swelling and swelling in the pelvis and legs can be a sign of pelvic varicose veins. This swelling may increase during the day and decrease by resting and elevating the legs.
- Sensitivity and pain when tapping: Tapping or pressing the pelvic area may increase sensitivity and pain in people with pelvic varicose veins.
- Fatigue and heaviness in the legs: Feeling more tired and heaviness in the legs may be due to a defect in the blood flow from the pelvic veins, which caused pelvic varicose veins.
- Appearance of protrusions and venous networks: Prominent pelvic veins and venous networks may be visible in the pelvic area.
If you experience any of these symptoms, visiting a specialist doctor can lead to a correct diagnosis and appropriate treatment plan. The doctor will determine the exact diagnosis and appropriate treatment by examining the symptoms, performing diagnostic tests and physical examination.
What people are affected by varicose veins of the pelvis?
Pelvic varicose veins can affect anyone, but certain factors and risk factors can make it more likely to occur. The following people are at the highest risk:
- Pregnant women: During pregnancy, hormonal changes, increased blood volume and pressure on the pelvic veins can lead to pelvic varicose veins.
- People with a family history of pelvic varicose veins: Genetics plays an important role in the occurrence of pelvic varicose veins, and if there is a family history of this condition, the likelihood of its occurrence increases.
- People who Have structural defects in the pelvic veins: Some people may be born with structural and functional defects in the pelvic veins that lead to pelvic varices.
- People who have chronic pressure in the pelvic area: Activities such as handling heavy objects, heavy loads on the pelvic area, or chronic pressure in the pelvic area can lead to pelvic varices.
- People with a history of seizures. Some people may develop pelvic varices after seizures, especially frequent and severe seizures. Risk factors: Factors such as obesity, sitting for long periods of time, lack of proper physical activity, taking anticoagulant pills, and drug use can increase the risk of pelvic varices. It is important to know that anyone can develop pelvic varices. but these factors can increase the probability of its occurrence. If you experience symptoms of pelvic varices or have similar risk factors, it is recommended to see a specialist doctor.

What are the complications of varicose veins of the pelvis?
Pelvic varicose veins can lead to various complications and problems. Some of the common complications of varicose veins of the pelvis are:
Inflammation and infection
Pelvic varices may cause inflammation and infection in the pelvic area. This problem is usually associated with pain, swelling, redness and sensitivity in the affected area.
Bleeding
Pelvic varicose veins can lead to bleeding in some cases. Bleeding may occur inside the pelvic area and be internal or transferred to the outside of the body.
Blood clot formation
Pelvic varicose veins can cause the formation of blood clots in the pelvic veins. These blood clots may lead to bleeding or if they are separated from their place, they are transferred to the pulmonary vessels and form a blood blockage in the lung (thrombus deviation), which is a serious health risk.
hard and painful parts in the pelvic region
Some varicose veins may be recognizable as hard and painful areas in the pelvic region. These parts usually may be more painful with pressure and treatment.
The occurrence of wounds caused by blood flow imbalance
Pelvic varices may cause ulcers in the pelvic area. These wounds are usually located in the area covering the skin and can be accompanied by pain, inflammation, and discharge.
If you experience any of these complications or complain of pelvic varicose veins, it is very important to see a specialist doctor. The doctor will determine the appropriate treatment plan by accurately diagnosing pelvic varices and checking its severity.
How are pelvic varicose veins diagnosed?
Diagnosis of pelvic varices is usually done by a vascular specialist and varicologist. To diagnose pelvic varices, the doctor may use the following methods and tests:
- Physical examination: The doctor collects important information by examining the pelvic area and asking about the symptoms and history of the disease. He or she may check to see if the pelvic veins are enlarged, narrowed, or swollen.
- Two-dimensional ultrasound (Duplex Ultrasound) This method uses sound waves to take pictures of the pelvic veins and shows the blood flow in these veins. With this method, the doctor can check the status and level of pelvic varices. Angiography In this method, radiopaque material enters the pelvic veins and then radiographic images are taken from them. This method is used less often and is usually used in more complex cases and more accurate diagnosis.
After diagnosing pelvic varices, the doctor can determine the next step of treatment. This may include changes in lifestyle, use of medications, pressure therapy, ultrasound with various imaging methods, lasers, and surgical procedures. It is important to consult a specialist doctor to determine the best treatment method for you.

how to treat varicose veins of the pelvis
Treatment for pelvic varices depends on several factors, including the severity of symptoms, the size and location of the varices, the individual's general health status, and the physician's preferences. Treatment of pelvic varices may include the following:
- Changes in lifestyle: Self-care measures such as changing the way you sit and stand, increasing regular physical activity, and exercises that strengthen the leg muscles (such as walking and swimming) can help reduce the symptoms of varicose veins. Also, avoiding some risk factors such as long periods of sitting and standing, high fat in the diet and using compression clothing can be useful. Using compression stockings for varicose veins can apply proper pressure to the pelvic veins and improve blood flow. These socks are available in different sizes and pressures and should be used according to the doctor's recommendation.
- Medications: Some medications can reduce the symptoms of pelvic varices and improve blood flow. The doctor may prescribe drugs such as non-steroidal anti-inflammatory drugs (NSAIDs), varicocetomies, and drugs that affect muscles and blood vessels.
- Ultrasound and imaging methods: In some cases, ultrasound with different imaging methods may be used. These methods include two-dimensional ultrasound, color Doppler ultrasound and three-dimensional blood flow ultrasound (3D Doppler). These methods help the doctor to examine the condition of pelvic varices more precisely and to determine the appropriate treatment. Surgical methods: In severe cases of pelvic varices or in case of failure to improve with non-surgical treatment methods, surgical methods to diagnose pelvic varices are usually performed by a specialized physician specializing in vessels and lubrication (varicose specialist). To diagnose pelvic varices, the doctor may use the following methods and tests:
- Physical examination: The doctor collects important information by examining the pelvic area and asking about the symptoms and history of the disease. He or she may check to see if the pelvic veins are enlarged, narrowed, or swollen.
- Two-dimensional ultrasound (Duplex Ultrasound) This method uses sound waves to take pictures of the pelvic veins and shows the blood flow in these veins. With this method, the doctor can check the status and level of pelvic varices. Angiography In this method, radiopaque material enters the pelvic veins and then radiographic images are taken from them. This method is used less often and is usually used in more complex cases and more accurate diagnosis.
After diagnosing pelvic varices, the doctor can determine the next step of treatment. This may include changes in lifestyle, use of stockings, medications, pressure therapy, ultrasound with various imaging methods, lasers, and surgical procedures. It is important to consult a specialist doctor to determine the best treatment method for you.
How is pelvic varicose physiotherapy performed?

Physiotherapy in the treatment of pelvic varicose veins can be used as one of the non-surgical methods along with other treatment methods. This method, by using exercises and physical methods, facilitates the improvement of blood flow and the symptoms of pelvic varicose veins. Below are some of the most important physical therapy methods for the treatment of pelvic varicose veins:
- Strengthening exercises: Exercises designed to strengthen the muscles of the legs and pelvic area can facilitate improved blood flow. These exercises can include standing exercises, walking, swimming, and resistance exercises using weights or scales. Also, relaxation and extension exercises can also be effective in reducing the symptoms of pelvic varices. Massage: Massaging the parts affected by pelvic varices can facilitate the improvement of blood flow and the reduction of related symptoms. Gentle massage with soft movements and appropriate pressure on the pelvic area can be useful. It is important that the massage is performed by a skilled physiotherapist who is aware of the condition of pelvic varicose veins. Compression Therapy Using varicose stockings or compression bandages during the day can improve blood flow and ease the symptoms of pelvic varicose veins. These socks and bandages apply appropriate pressure on the pelvic area and improve blood flow. Water therapy: Using water therapy such as hot and cold baths and hydrotherapy can improve blood flow and reduce the symptoms of pelvic varicose veins. The use of hydrotherapy should be done under the supervision of a specialist physiotherapist.
- Education and life advice: The physiotherapist may advise you on how to best sit and stand during the day. Also, he may make recommendations about weight control, increasing physical activity, using appropriate clothing and preventing the occurrence of risk factors such as sitting or standing for a long time. He can set up a suitable treatment plan for you and teach you the right exercises and methods to reduce the symptoms of pelvic varicose veins. Also, the physiotherapist can use other methods such as electrotherapy, laser therapy or the use of other special devices to speed up recovery.
Endnote
Physiotherapy plays a very important role in improving and treating pelvic varices. Physiotherapy includes strengthening and flexibility exercises and techniques that accelerate recovery and help reduce symptoms and pain. Usually, the physiotherapist will prescribe specific exercises for you to do on a regular basis. شما می توانید با کلینیک تخصصی رادین تماس حاصل فرمایید تا با رزرو وقت با همکاری کادر مجرب مجموعه به بهبود خود با تکنیک ها و مجهزترین تجهیزات سرعت بخشید.
همچنین میتوانید از خدمات فیزیوتراپی واریس لگن با بیمه آسیا نیز بهرمند شوید.