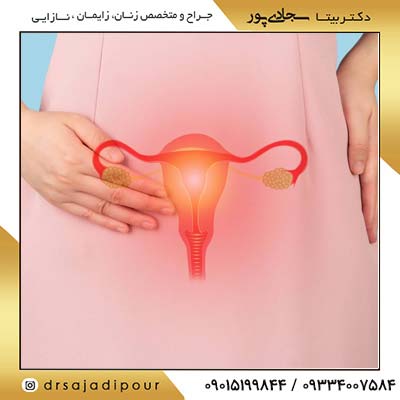
برداشتن تخمدان یا اووفورکتومی (Oophorectomy) به عمل جراحی برداشتن یکی یا هر دو تخمدان گفته میشود. This procedure may be performed for various medical reasons. Dr. Bita Sajjadipour
Conditions of oophorectomy
Some conditions and reasons that may require oophorectomy include:

- Ovarian cancer: One of the most common reasons for oophorectomy is the treatment of ovarian cancer. In this case, the surgeon may remove the ovaries to prevent the spread of cancer.
- Ovarian cysts or tumors: If noncancerous cysts or tumors develop in the ovaries and cause pain or other problems, oophorectomy may be the treatment of choice.
- Endometriosis: In some cases, if endometriosis (a condition in which tissue similar to the uterus grows outside (the uterus grows) damage the ovaries, oophorectomy may be a solution to reduce pain and prevent further problems.
- Chronic infections or damage to the ovaries: If the ovaries are seriously affected due to infection or chronic damage, they may be removed for treatment.
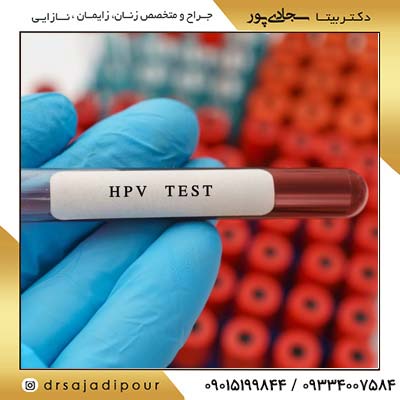
- Cancer prevention in hereditary cases: Some women who have certain genetic mutations, such as BRCA1 or BRCA2 mutations, may undergo preventive oophorectomy because of their high risk of developing ovarian cancer.
- Surgeries related to hormonal changes: Sometimes an oophorectomy is performed to treat hormonal problems such as adrenal hyperplasia or other disorders that arise from the ovaries.
Reasons for needing to remove ovaries
According to mayoclinic
Ovarian tube abscess. Fallopian tube abscess is a pus-filled pocket that contains a fallopian tube and an ovary.
- A tubo-ovarian abscess. A tubo-ovarian abscess is a pus-filled pocket involving a fallopian tube and an ovary.
- Endometriosis.
- Noncancerous ovarian tumors or cysts.
- Ovarian cancer.
- Ovarian torsion.
- Reducing cancer risk.
- Endometriosis.
- Non-cancerous ovarian tumors or cysts.
Ovarian cancer.- Torsion of the ovary.
- Reducing the risk of cancer.

Ovarian removal surgery
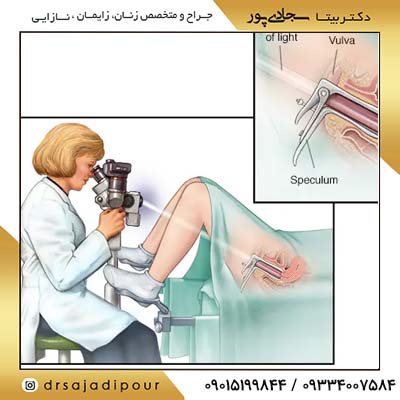
There are different methods for removing the ovaries (oophorectomy) and the doctor chooses the best option based on the patient's condition and the reason for the surgery. The most important methods are:
- Laparoscopy:
In this method Minimally invasive, the surgeon removes the ovary through small incisions in the abdomen and with the help of a camera and special tools.- Advantages:
- faster recovery period
- Less pain and wound
- Less risk of infection
- Disadvantages:
- In very complicated cases, there may be a need to convert to open surgery.
- Open surgery (laparotomy):
In this procedure, the surgeon makes a larger incision in the abdomen to gain access to the ovaries.- Advantages:
- Possibility of better access to tissues in complex cases (such as advanced cancer)
- Disadvantages:
- Longer recovery period
- More pain and higher risk of infection
- Through the vagina (vaginal oophorectomy):
In certain cases, the ovaries can be removed through an incision in the vaginal wall, but this is less common.- Advantages:
- There is no wound on the skin of the abdomen
- Disadvantages:
- It may not be suitable for some clinical conditions.
choosing the best surgical method oophorectomy
The decision about the type of surgery depends on several factors, including the reason for the removal of the ovary (eg, cancer, cyst, or prophylaxis), the patient's general health, and the surgeon's experience and advice. For example, if a patient has ovarian cancer, open surgery is usually preferred for closer inspection of the tissues. In contrast, for simple cysts or preventive surgeries, laparoscopy is more commonly used. Dr. Bita Sajjadipour Best Gynecologist in Chitgar is your guide in this regard.

General advantages and disadvantages of removing the ovaries
The general advantages and disadvantages of removing the ovaries are:
| Advantages | Disadvantages |
| Treatment of serious diseases such as cancer or ovarian torsion | The possibility of early menopause symptoms (hot flashes, bone loss, mood changes) |
| Reducing the risk of some diseases (such as ovarian cancer) in preventive cases | The need to adjust hormones in some cases |
| Common risks of surgery (infection, bleeding, anesthesia problems) |
Finally, the doctor suggests the best option according to the individual conditions of the patient and the advantages and disadvantages of each method.
Complications of ovary removal
Removing the ovaries (oophorectomy) can have short-term and long-term side effects. Some of these complications are related to the surgery itself, and others are related to hormonal changes after removing the ovaries. Being aware of these complications and their management methods will help the patient to have a better recovery and maintain his quality of life.
Short-term effects:
- Pain and discomfort after surgery
- Bleeding and wound infection
- Anesthesia effects (such as nausea and vomiting)
- Damage to adjacent organs
Long-term side effects (especially in bilateral removal of ovaries):
- Premature menopause:
Removal of the ovaries before menopausal It naturally reduces estrogen and progesterone hormones. This can lead to hot flashes, vaginal dryness, decreased libido, mood swings, and decreased bone density.- Management:
- Hormone therapy (HRT) if the patient's condition is suitable.
- Using vaginal lubricants or moisturizers to relieve dryness.
- Performing weight bearing exercises and taking calcium and vitamin D supplements to strengthen bones.
- Increased risk of cardiovascular diseases:
Estrogen deficiency may increase the risk of heart diseases.- Management:
- maintain proper weight.
- Healthy diet and regular physical activity.
- Control of blood pressure and cholesterol.
- Mood changes and depression:
A sudden decrease in hormones can cause mood swings or even depression.- Management:
- Psychological or psychiatric consultation.
- Antidepressants if needed.
- Relaxing activities such as yoga, meditation, or breathing exercises.

Essential care after surgery oophorectomy
Essential care after oophorectomy surgery includes:
- Rest and activity limitation:
- In the early days, avoid heavy activities, lifting heavy objects and vigorous sports.
- After a few days, start light activities and gradually increase the amount of activity.
- Pain Management:
- The doctor usually prescribes painkillers. این داروها را طبق دستور مصرف کنید و در صورت کاهش درد، به تدریج دوز آنها را کاهش دهید.
- استفاده از کیسهی گرم روی نواحی شکم (با دستور پزشک) میتواند به کاهش درد و گرفتگی کمک کند.
- رعایت بهداشت زخم:
- زخمهای جراحی را طبق دستور پزشک تمیز و خشک نگه دارید.
- در صورت وجود پانسمان، از دستکاری آن خودداری کرده و در زمان تعیینشده تعویض کنید.
- از غوطهور شدن در آب (مانند استخر یا وان) تا زمانی که پزشک اجازه نداده است، پرهیز کنید.
- مصرف داروها و مکملها:
- آنتیبیوتیکها یا داروهای دیگری که پزشک تجویز کرده است را کامل مصرف کنید.
- در صورت نیاز به هورموندرمانی یا مکملهای کلسیم و ویتامین D، طبق دستور پزشک عمل کنید.
- رژیم غذایی و هیدراتاسیون:
- مصرف مایعات کافی و یک رژیم غذایی متعادل میتواند به بهبودی سریعتر کمک کند.
- از غذاهای پرچرب و سنگین که ممکن است باعث نفخ یا ناراحتی شکمی شوند، پرهیز کنید.

چه زمانی باید به پزشک متخصص مراجعه کرد؟
- افزایش دمای بدن:
اگر تب (بالاتر از ۳۸ درجه سانتیگراد) دارید یا احساس لرز میکنید، این ممکن است نشانه عفونت باشد. - قرمزی، ورم یا ترشح غیرطبیعی از زخم:
- اگر زخم جراحی قرمز، متورم یا دچار ترشح چرکی شود، به پزشک اطلاع دهید.
- درد شدید و غیرمعمول:
- اگر درد به جای کاهش، شدیدتر شود یا با داروهای تجویز شده کنترل نشود، نیاز به بررسی دارد.
- مشکلات ادراری یا گوارشی:
- اگر دچار مشکل در دفع ادرار، تغییرات غیرمعمول در حرکات روده، یا درد شدید شکمی شدهاید، به پزشک مراجعه کنید.
- ضعف شدید، سرگیجه یا بیحالی:
- اگر احساس ضعف شدید دارید یا توان انجام فعالیتهای روزمره را ندارید، ممکن است به کمک پزشکی نیاز داشته باشید.
- تورم و درد در پاها:
- اگر پاهای شما دردناک، قرمز یا متورم شدند، این میتواند نشانهی لختهی خون باشد و باید بلافاصله بررسی شود.
نتیجهگیری
رعایت دستورالعملهای پزشک، نظارت دقیق بر علائم، و مراجعه به پزشک در صورت بروز نشانههای نگرانکننده، میتواند به بهبودی سریعتر کمک کرده و از عوارض احتمالی جلوگیری کند.


![The role of inositol in the treatment of female infertility [obstetrics and gynecology specialist]](/storage/posts/covers/2026/01/05/c0b071d7095fdcbaa34903c34e092d27a7f5b2fc471de3ff89c0a6eb0c446a10.jpg)

![Children's vaginal infection: symptoms and treatment [obstetrics and gynecology specialist]](/storage/posts/covers/2026/01/05/e56f480f09acfaf71854a94f42ccf293be7e378bd9a4adcffd54d5476bf51caa.jpg)

![Breast cancer [breast] symptoms, diagnosis + treatment [gynecologist]](/storage/posts/covers/2026/01/05/0d2c008b72cfbf5343598c8045fd73cdfbfe6a0e567bd035ea8e1fc90702e96a.jpg)



![Vaginal infection in pregnancy: symptoms, diagnosis and treatment [obstetrician and gynecologist]](/storage/posts/covers/2026/01/05/74fbd328a8a4a83f39778f4a417048ddeb814f527d50d1afc9e23bbe0ad5e371.jpg)